Respiratory distress syndrome (RDS) – Health of the children has been considered as the vital importance to all societies because children are the basic resource for the future of humankind. Nursing care of children is concerned for both the health of the children and for the illnesses that affect their growth and development. The increasing complexity of medical and nursing science has created a need for special area of child care, i.e. pediatric nursing.
Pediatric nursing is the specialized area of nursing practice concerning the care of children during wellness and illness. It includes preventive, promotive, curative and rehabilitative care of children. It emphasizes on all round development of body, mind and spirit of the growing individual. Thus, pediatric nursing involves in giving assistance, care and support to the growing and developing children to achieve their individual potential for functioning with fullest capacity.
Respiratory distress syndrome (RDS)
Respiratory distress syndrome (RDS):
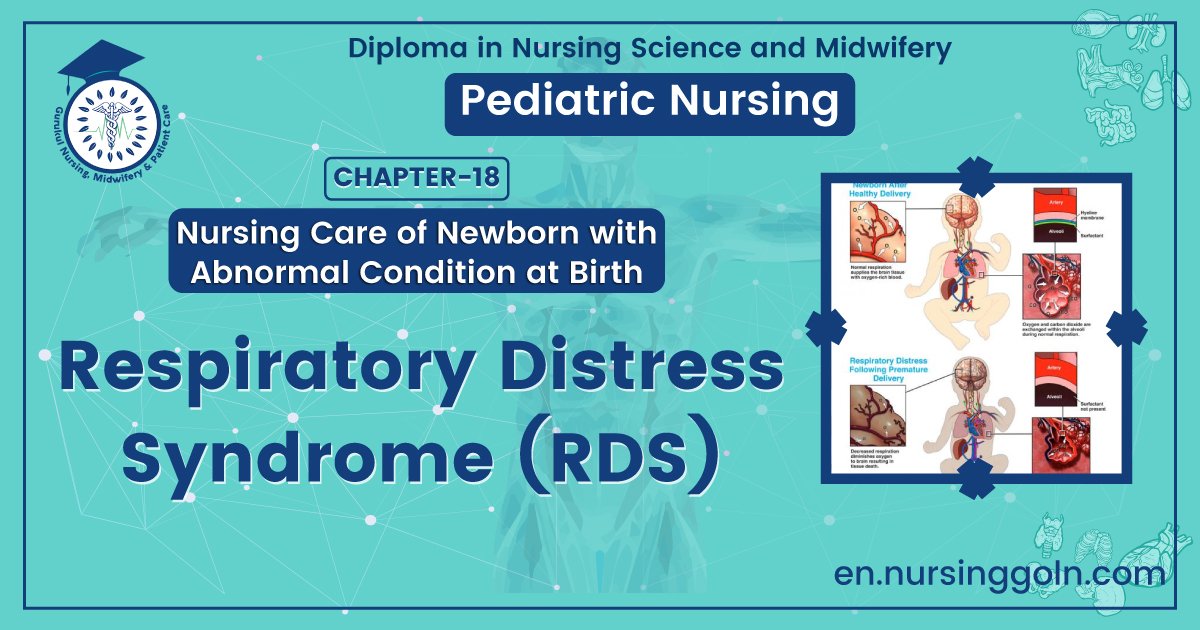
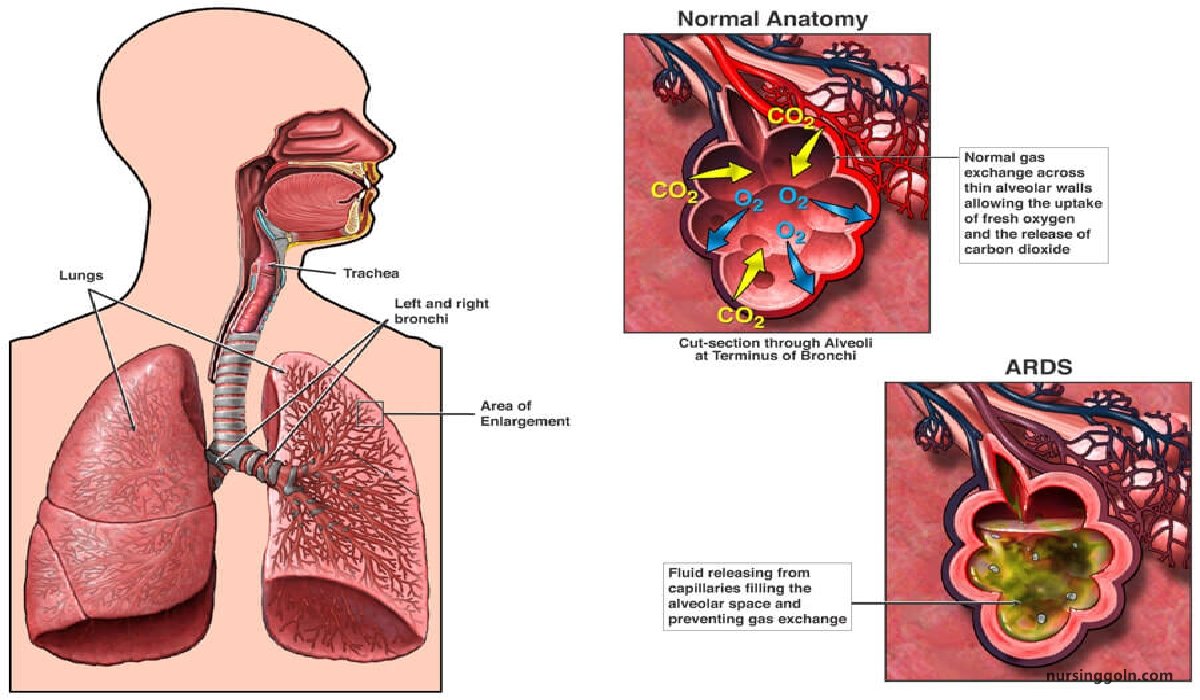
Respiratory distress syndrome (RDS) is the most common cause of respiratory disease in preterm neonates. The disease manifests as surfactant deficiency characterized by collapsed alveoli and low lung volume.
[Ref-Annamma Jacob/2/245]
Or,
Neonatal respiratory distress syndrome (RDS) is a problem often seen in premature babies. The condition makes it hard for the baby to breathe.
Or,
Respiratory distress syndrome (RDS) is a breathing disorder that affects newborns. RDS rarely occurs in full-term infants. The disorder is more common in premature infants born about 6 weeks or more before their due dates.
[Ref-www.nhlbi.nih.gov]
Risk factors of respiratory distress syndrome of a newborn:
1. Prematurity
2. Other risk factors include-
- Multi-fetal pregnancies.
- Maternal diabetes.
- Cesarean section.
- Asphyxia & Hypothermia.
[Ref-Piyush Gupta/1/238]
Causes of respiratory distress syndrome:
| Maternal causes |
|
| Cardiac cause |
|
| Pulmonary cause |
|
| Obstructive cause |
|
| Neurologic cause |
|
[Ref-Suraj Gupta/11/216]
Clinical features of RDS:
1. Tachypnea (respiratory rate > 60/minute) appears immediately or within six hours after delivery.
2. Another characteristic feature of RDS is the expiratory grunt.
3. Cyanosis appears, as hypoxia ensues.
4. Atelectasis and respiratory failure are characterized by –
- Lethargy
- Irregular breathing and
- Apnea.
Interpretation:
1. A score of <5 indicates mild RD.
2. A score of 5 to 8 indicate moderate RD.
3. A score of 8 indicate severe RD.
Management of RDS in a newborn:
1. Maintaining of thermoneutral environment to keep the baby warm with normal body temperature.
2. Providing clear airway by positioning and removal of secretions by suctioning
3. Administering oxygen by oxygen hood or nasal prongs to maintain target saturations. spoz levet should be maintained for term neonates 90 to 93 percent and for preterm neonates 88 to 92 percent. Arrangement to be kept ready for respiratory support by CPAP (Continuous Positive Pressure Ventilation) or by invasive mechanical ventilation in case of impending respiratory failure.
4. Continuous monitoring of neonates general conditions, respiratory status (respiratory rate, retractions, grunting, cyanosis, nasal, flaring), heart rate, body temperature, SpO2 CRT, BP, blood gas, and other parameters.
5. Giving IV fluid therapy and maintaining normal blood glucose and calcium level.
6. Treating apne4 if present, with PPV (Positive Pressure Ventilation) using resuscitation bag and mask or endotracheal tube and resuscitation bag. Drugs (Aminophylline or Caffeine Citrate) may be required to treat apnea in some cases.
7. Antibiotic therapy may be needed to treat sepsis, if present.
8. Surfactant therapy is now recommended as the treatment of choice in preterm neonates with moderate to severe RDS.
9. Insertion of orogastric tube to be done to decompress the stomach during respiratory distress.
10. Initiation of gavage feeding to be done with minimal amount of EBM, when the respiratory distress subsides.
11. Gradually paladai or katori-spoon feeding to be started and then to be shifted to breast feeding when the baby is comfortable to suck and swallow.
12. Providing routine care and practicing infection control measures.
13. Arrangement of cause-specific management to be done to promote better prognosis. Surgical interventions should be planned as emergency or elective operations depending upon the nature of problems.
14. Details records and reports to be maintained.
15. Discharge planning and teaching to the mother and family members should be done for home care and follow up.
[Ref-parul Datta/34/86, 87]
Nursing care of newborn with RDS:
Assessment:
1. Perinatal history.
2. Signs of respiratory distress, including tachypnea, apnea, retractions, nasal flaring, and grunting.
3. Assess breath sounds.
4. Assess cardiovascular system including determining the heart rate and noting any murmur.
5. Evaluate the results of laboratory test.
Nursing diagnosis & planning:
1. Impaired gas exchange related to immaturity of the lungs and chest wall and/or insufficient amounts of surfactant
2. Ineffective airway clearance related to obstruction or inappropriate positioning of an endotrachial tube
3. Ineffective breathing pattern related to asynchronous breathing between the infant and the ventilator, ventilator malfunction, or inappropriate ventilator support.
4. Monitor infant’s vital signs, respiratory status blood gas and pulse oximetry are also done for evidence of respiratory distress
5. Suctioning of the endotracheal tube as needed to optimize ventilation
6. Monitor respiratory support to ensure synchronous breathing between the ventilator and infant.
7. Encourage the parents to verbalize fear and concerns as well as participating in caring.
Interventions:
1. Monitor infant’s vital signs, respiratory status blood gas and pulse oximetry are also donefor evidence of respiratory distress.
2. Proper positioning of the infant, the prone position or supine with the neck slightly extended and the nose pointed toward the ceiling to prevent narrowing of the airway.
3. Suctioning of the endotracheal tube as needed optimizes ventilation.
4. Monitor respiratory support to ensure synchronous breathing between the ventilator and infant.
5. Encourage the parents to verbalize fear and concerns as well as participating in caring.
Evaluation:
1. Does the infant maintain normal oxygen saturations on pulse oximetry?
2. Does the infant maintain a normal respiratory rate?
3. Are the infant’s breath sounds and chest wall movements adequate and equal bilaterally?
4. Are the infant’s blood gases within normal limits?
5. Are ventilator setting adjusted in a timely manner whenever blood gas results fall outside established parameters?
[Ref-Dr.Tanvir/Newborn Nursing/4th/]
Complications of RDS:
1. Intraventricular haemorrhage.
2. Bronchopulmonary dysplasia.
3. Pulmonary haemorrhage.
4. Retrolental fibroplasias.
5. Neurological abnormalities.
6. Infection.
7. Patent Ductus Arteriosus (PDA).
8. Apnoea.
[Ref-Annamma Jacob/2/469]
Prevention of RDS in newborns:
1. Avoid premature delivery to prevent lung immaturity
2. Give prenatal steroid (betamethasone, dexamethasone) to enhance lung maturity.
3. Give surfactant to premature infants soon after birth or after first few hours of life.
[Ref-Suraj Gupta/11/217]