Septic arthritis -An orthopedic nurse is a nurse who specializes in treating patients with bone, limb, or musculoskeletal disorders. Nonetheless, because orthopedics and trauma typically follow one another, head injuries and infected wounds are frequently treated by orthopedic nurses.
Ensuring that patients receive the proper pre-and post-operative care following surgery is the responsibility of an orthopedic nurse. They play a critical role in the effort to return patients to baseline before admission. Early detection of complications following surgery, including sepsis, compartment syndrome, and site infections, falls under the purview of orthopedic nurses.
Septic arthritis
Definition of septic arthritis:
Septic arthritis is defined as the bacterial infection of the joint, which causes an intensive inflammatory reaction with migration of polymorpho- nuclear leucocytes and subsequent release of proteolytic enzyme which could leading to destruction of articular cartilage and later the joint.
[Ref-John Ebnezar, Textbook of orthopedics, 4 edition P. 575]
Or
Septic arthritis may be defined as the invasion of the joint cavity with microorganisms.
[Ref- Lippincott, Adult orthopedic nursing, P-66]
Or
Septic arthritis is a medical emergency. It is the most rapid and destructive disease, and has significant morbidity and a mortality of 10%.
[Ref- Davidson’s “Principles & Practice of Medicine” 21″ edition, page-1103]
Or
Histologic definition, when WBC count in the synovial fluid is greater than 50,000 with 75% polymorphic neutrophils and negative lyme titre.
[Ref-John Ebnezar, Textbook of orthopedics, edition P-575]
Causative organisms responsible for the septic arthritis: They are most common offending organisms are-
1. Staphylococcus aureus(50%).
2. Streptococcus(20%).
3. Pneumococcus(10%).
4. Gonococcus
5. E.Coli
6. H.influenzae. (common in children)
[Ref-John Ebnezar, Textbook of orthopedics, edition,P-575]

Pathological changes in septic arthritis:
The usual triggers is a haematogenous infection which settles in the synovial membrane, there is an acute inflammatory reaction with a serious or sero purolent exudates and an increase in synovial fluid As pus appears in the joints, articular cartilage is eroded and destroyed, partly by bacterial enzymes and partly by proteolytic enzymes released from synovial cells, inflammatory cells, pus.
In infants the entre epiphysis which is still largely cartilaginous, may be severly damaged. In older children, vascular occlusion may lead to necrosis of the epiphyseal bone. In adults the effects are usually confined to articular cartilage, but in late cases there may be extensive erosion due to synovial proliferation and in growth.
If the infection is untreated, it will spread to the underlying bone or brust out of the joint to form abscess and sinuses.
Routes of entry of organisms for Pyogenic arthritis:
Easy to remember 5P s –
1) Primary focus in respiratory system, GIT etc.
2) Pyogenic osteomyelitis.
3) Punctured wound.
4) Pneumonia.
5) Primary focus in joint.
Joint may be infected: A join may be infected by followings
1) Direct invasion through a penetrating wound.
2) Intra articular injection or arthroscopy.
3) Direct spread from an adjacent bone abscess.
4) Blood spread from distant side.
[Ref-Apleys System of orthopedic and fractures, 19th edition, P-43]
Risk for septic arthritis:
1) Age:
a) Young age (Caused by H. influenza).
b) Elderly adults (Caused by Gonococcus).
2) Trauma:
a) Open fracture.
b) Punctured wound..
3) Pre existing joint diseases:
a) Rheumatoid arthritis (RA).
b) Osteomyelitis
4) DM.
5) Malignancy.
6) Prolonged steroid therapy.
7) AIDS patients.
[Ref- Apleys, System of orthopedic and fractures, 19h + John Ebnezar, Textbook of orthopedics, edition]
Common joints involved in case of pyogenic arthritis:
A) In adults:
a) Knee (53%)
b) Hip (20%)
c) Elbow (17%)
d) Shoulder (10%)
B) In Children:
a) Knee (39%)
b) Hip (32%)
[Ref-John Ebnezar, Textbook of orthopedics, edition P-575]
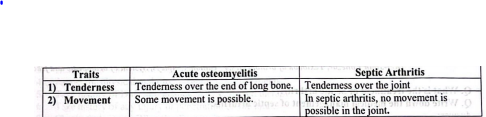
Difference between Acute osteomyelitis and septic arthritis:
Clinical features of septic arthritis:
A. History:
a) Open fracture.
b) Puncture wound.
c) Age.
d) Patients having DM, Rheumatoid arthritis,Steroid therapy.
B. Manifestation:
1) Symptoms:
a) Sever joint pain usually mono -articular (90% cases)
b) Joint swelling – commonly in knee and hip.
e) Restricted movement-pain increase when joint is moved.
d) Fever-mild rise of body temperature.
2) Signs:
a) Single joint involved.
b) Joint become Hot swollen, tender, redness.
c) Joint swollen – over the joint not end of lonf bone.
d) Deformity Patient complaints that flexion deformity.
e) Painful joint-pain increase on active movement on joint.
[Ref-John Ebnezar, Textbook of orthopedics, edition, Apleys System of orthopedic and fractures,19]
Investigation will you done to confirm the diagnosis of Septic arthritis:
1) X-Ray of the Joint: For septic arthritis findings are,
a) Soft tissue swelling.
b) Loss of tissue plane.
c) Slight sublaxation.
d) Narrowing of the joint spaces.
2) MRI (Magnetic Resonance Imaging).
3) Aspiration of synovial fluid: Often found
a) Turbid and blood stained
4) Synovial fluid analysis:
Accurate diagnostic tools tested for cells, sugar and proteins,
a) Synovial fluid culture+ve
b) Gram stain = +ve.
c) Leucocyte count > 50,000 per ml suggestive to sepsis.
5) Blood:
a) WBC Increased (50,000-1,00,000)
b) ESR Increased
c) Hb% Decreased.
6) CRP (C-Reactive protein):
Increased (>10mg/dl)
[Ref-John Ebnezar, Textbook of orthopedics, edition + Apleys, System of orthopedic and fractures, 19″]

A) General Supportive care:
1) Analgesics-to relief pain of joint.
2) Splintage -Rest or immobilize the joint by POP (Plaster of paris).
3) Traction-if necessary when there is chance of dislocation.
4) Antibiotics: Flucloxacillin 2 gm I/V 6 hourly.
5) Larry our proper investigation.
B) Surgical:
1) Drainage: Under anaesthesia the joint is opened through a small incision, drained and washed out with normal saline.
2) Arthrotomy: when severely affected the joint
(Ref-John Ebnezar Textbook of orthopedics, edition P-576+ Apleys System of orthopedic and fractures, 19 P-44)
Complication of septic arthritis:
1) Avascular necrosis.
2) Joint destruction.
3) Pathological dislocation (Hip dislocation).
4) Slight sublaxation.
5) Osteoarthritis in later year.
6) Acute osteomyelitis
7) Septicaemia/ Pyaemia.
8) Partial or complete destruction of epiphysis.
9) Deformity of the joint.
10) Acetabular dysplasis.
11) Articular cartilage erosion (Chondrolysis)
12) Pseudoarthrosis of hip.
13) Complete ankylosis of the joint.
14) Coxa Vera.
15) Osteoporosis.
16) Post infection arthritis.
17) Amyloidosis.
[John Ebnezar, Textbook of orthopedics, 4 edition p-577+ Apleys System of orthopedic and fractures, 19″ P. 43]
Nursing management of septic arthritis:
A) Assessment:
1. Assess painsites, severity, radiation, cause
2. Assess joint movement for is it restricted?
3. Assess joint hot, swollen, tender,
4. Assess the physical mobility of septic arthritis patients.
5. Take history of DM, Malignancy, AIDS, Steroid therapy.
6. Take history of any injury or penetration on the joint.
7. Check vital signs BP, pulse Respiration, temperature.
8. Observe mental condition of the patients.
9. Assess the level of knowledge about care
B) Nursing diagnosis:
1) Acute pain related to inflammation of the joint.
2) Impaired physical mobility related to movement increase pain.
3) Increase of body temperature related to infection in the joint.
4) Risk of development of secondary infection due to inadequate care.
C) Nursing intervention:
1) Relief of pain:
a) Keep the patients in comfortable position…
b) Avoid unusual movement of joint.
c) Aspiration of synovial fluid to decrease suppuration.
d) Avoid weight bearing activity in the limb.
e) Warm compress help to control pain.
f) Administer analgesics according to doctors order.
2) Immobilization of the joint:
a) Keep the patients in complete bed rest
b) Immobilize the limbs with cast.
c) Explain the benefit of plastering.
d) Avoid the tight fitting cast.
e) Regular observation of the cast.
f) Never give full plaster over the swellings.
g) Passive exercise is done by nurse or physiotherapist on the affected joint to prevent contracture.
h) When acute phase is over patients is encourage to ambulation.
i) Encourage him to do active exercise on legs. E.g. Flexion, extension, medial rotation, lateral rotation.
3) Reducing body temperature.:
a) Measuring body temperature and record in temperature chart.
b) Encourage to take plenty of fluid.
c) Provide cold sponging with permission of patients d) Give antipyretic drugs according to doctor orders.
4) Prevention of infection:
a) Aspiration of synovial fluid for culture to find out causative organisms.
b) Provide cleanliness around the joint.
c) Draining of pus and washing the joint with normal saline.
d) Use of clean, sterile instrument during aspiration.
e) If punctured wound present provide aseptic technique.
f) Regular observation of TC, DC, ESR, C-RP etc.
g) General care towards invasive line such as i/v line, Catheter, drainage area.
h) Give antibiotic according to doctors order.
Differential diagnosis of Septic arthritis
1. Acute osteomyelitis
2. Haemarthrosis.
3. Juvenile Rheumatoid arthritis.
4. Gout and pseudogout.
5. Rheumatic fever.
[Ref-Apleys, System of orthopedic and fractures, 19 Page-43]
a) Possible diagnosis: Septic arthritis.
b) Differential Diagnosis: Please see above.
c) Justification of septic arthritis: Justifications are

1) In case of acute osteomyelitis:
a) Tenderness is over the end of long bone (NOT over the joint)
b) Some degree of movement is possible (No limitation). = So not acute osteomyelitis.
2) In case of haemarthrosis:
a) Haemophilic patients
b) Bleeding into joint.
c) H/o bleeding during brushing teeth, d) Signs of bleeding into calf muscle. = So this case is not a Haemarthrosis.
3) In case of juvenile Rheumatoid arthritis:
a) Involved in small joint (Septic arthritis in large joint).
b) Swan neck deformity present (In this patients no swan neck deformity). =So this case is not Juvenile rheumatoid arthritis.
4) Rheumatic fever :
a) Migratory poly arthritis (But in septic mono- articular involvement)
b) Cardiac diseases present.
c) Age 5 years. = So this case is not rheumatic fever.
5) In Septic arthritis:
a) Tenderness over the joint
b) One joint become involved.
c) No movement is possible in involved joint.
6) Justification analysis: Analysis of D/D, revealed that above case is Septic arthritis.
[Ref- Apleys System of orthopedic and fractures, 19, Page-45]
