Shoulder dystocia – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Shoulder dystocia
Definition:
Shoulder dystocia refers to a situation where, after delivery of the head, the anterior shoulder of the fetus becomes impacted on the maternal pubic symphysis, or (less commonly) the posterior shoulder becomes impacted on the sacral promontory.
It is an obstetric emergency, with an incidence of approximately 0.6-0.7% in all deliveries. In this article, we shall look at the risk factors, clinical features and management of shoulder
dystocia.
Pathophysiology:
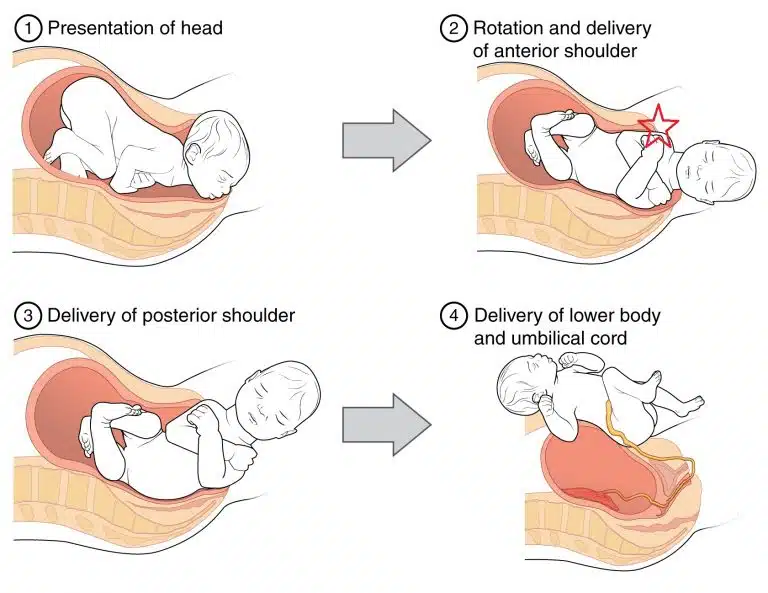
In normal labour, the fetal head is delivered via extension out of the pelvic outlet. This is followed by restitution of the fetal head, so it lies in a neutral position in relation to its spine. This means the fetal shoulders now lie in an anterior-posterior position.
Shoulder dystocia occurs when there is impaction of the anterior fetal shoulder behind the maternal pubic symphysis, or impaction of the posterior shoulder on the sacral promontory. A delay in delivery of the fetal shoulders leads to hypoxia in the fetus, proportional to the time delay to complete delivery.
Applying traction on the fetal head can result in fetal brachial plexus injury, and is major cause for litigation in obstetrics.
Risk Factors:
The risk factors for shoulder dystocia can be divided into pre-labour and intrapartum factors:
| Pre-Labour | Intrapartum |
|
|
Clinical Features:
Shoulder dystocia is defined by a delay in delivery of the shoulders following the head during a vaginal delivery with the next contraction after using normal traction.
- On examination, signs that may occur to aid the diagnosis are:
- Difficulty in delivery of the fetal head or chin.
- Failure of restitution the fetal remains in the occipital-anterior position after delivery by extension and therefore does not ‘turn to look to the side’.
- “Turtle Neck’ sign the fetal head retracts slightly back into the pelvis, so that the neck is no longer visible, akin to a turtle retreated into its shell.
Management
REMEMBER – If managed appropriately the risk of permanent brachial plexus injury can be almost eliminated.
The immediate steps in the management of shoulder dystocia include:
- Call for help – shoulder dystocia is an obstetric emergency (will need senior obstetrician, senior midwife and paediatrician in attendance).
- Advise the mother to stop pushing this can worsen the impaction.
- Avoid downwards traction on the fetal head (increases risk of brachial plexus injury) only use “routine” axial traction (i.e. keep the head in line with the baby’s spine), and do not apply fundal pressure (increases the risk of uterine rupture).
- Consider episiotomy – this will not relieve obstruction but can make access for manoeuvres easier.
- First Line Manoeuvres
- McRoberts manoeuvre – hyperflex maternal hips (knees to chest position) and tell the Act patient to stop pushing. This widens the pelvic outlet by flattening the sacral promontory and increasing the lumbosacral angle. This single manoeuvre has a success rate of about 90% and is even higher when combined with ‘suprapubic pressure’, (see below).
- Suprapubic pressure is applied in either a sustained or rocking fashion to apply pressure behind the anterior shoulder to disimpact it from underneath the maternal symphysis.
Second Line (“Internal) Manoeuvres
- Posterior arm – insert hand posteriorly into sacral hollow and grasp posterior arm to deliver.
- Internal rotation (“corkscrew manoeuvre”) – apply pressure simultaneously in front of one shoulder and behind the other to move baby 180 degrees or into an oblique position. If the above manoeuvres fail then roll patient onto all fours and repeat (this may widen the pelvic outlet as the legs are abducted and flexed).
Further Manoeuvers
These are only to be considered when the above measures have been unsuccessful, and are very rarely used in the UK:
- Cleidotomy – fracturing the fetal clavicle.
- Symphysiotomy – cutting the pubic symphysis.
- Zavenelli – returning the fetal head to the pelvis for delivery of the baby via caesarean section.
Post-Delivery
After delivery of the fetus, active management of the 3rd stage of labour is recommended (due to increased risk of PPH). A PR examination should be performed to exclude a 3rd degree tear. Shoulder dystocia can be a traumatic experience, particularly if the women does not have regional anaesthesia. Debrief the mother and birth partner(s), and advise them of the risk of recurrence with any subsequent delivery.
Consider a physiotherapist review before discharge, as women are at increased risk of pelvic floor weakness/3rd degree tear, musculoskeletal pain and temporary nerve damage. Additionally, a paediatric review is recommended before discharge to assess for brachial plexus injury, humeral fracture or hypoxic brain injury.

Complications
The complications of shoulder dystocia can be divided into maternal and fetal:
- Maternal – 3rd or 4th degree tears (3-4%), post-partum haemorrhage (11%).
- Fetal – humerus or clavicle fracture, brachial plexus injury (2-16%), hypoxic brain injury.