Third Stage Of Labor – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Third Stage Of Labor
3rd stage of labor:
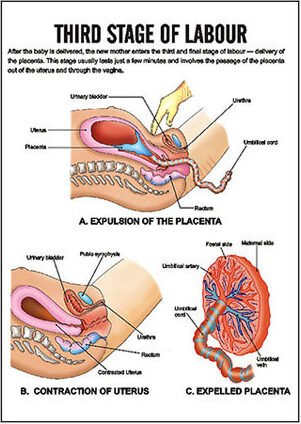
Third stage of labor extends from delivery of the foetus up to the delivery of placenta and membranes.
Or
Third stage of labor: The part of labor from the birth of the baby until the placenta (afterbirth) and fetal membranes are delivered. The third stage of labor is also called the placental stage.
Sign and symptoms /Criteria of 3rd stage of labor:
1. Pain: For a short time, the pt. experience no pain. Immediately following expulsion of the foetus, mother feels a sign of relief.
2. Before separation of placenta:
A. Per abdomen-
a. Uterus becomes, firm, non ballotable.
b. Fundal height reaches slightly below umbilicus.
B. Per vagina-
a. There may be slight trickling of blood.
b. Length of umbilical cord as visible from outside, remain static.
3. After separation of placenta:
A. Per abdomen –
a. Uterus becomes globular, firm contracted
b. Fundal height is slightly raised.
c. Slight bulging in supra pubic region
B. Per vagina-
a. Gush of vaginal bleeding
b. Permanent lengthening of the cord
4. Expulsion of placenta & membranes:
a. Marked retraction reduces effectively the surface area at the placenta about its half.
b. But as the placenta is inelastic, it cannot keep pace with such an extent of diminution resulting in its buckling.
c. A shearing force is instituted between the placenta & the placenta site which bring about its ultimate separation.
d. The plane of separation runs through deep spongy layer of deciduas basils so that a variable thickness of decides covers the maternal surface of the separated placenta.
Management of third stage of labor:
There are two types of management of third stage of labor;.
A. Expectant management
B. Active management
A. Expectant management:
1. Delivery of the baby.
2. Clamping and cutting of the umbilical cord.
3. Constant monitoring is mandatory and the patient should not be left alone.
4. Provide psychological support to the mother.
5. If the mother is delivered in the lateral position, she should be changed in the dorsal. position to note the features of placental separation and to assess the amount of blood loss.
6. Wait & watch for sign of placental separation.
7. Wait & watch for sign of placental separation.
8. Wait for spontaneous expulsion of placenta with the aid of gravity.
9. If fails, assisted expulsion is done by
➤ Inj-oxytocin, 5-10 unit IV or IM
➤ If fails, control cord traction & fundal pressure
10. Examination of placenta, membrane and umbilical cord.
11. Inspection of the vulva, vagina and perineum is done.
B. Active management:
Active management of third stage of labor includes;
➤Immediate oxytocin
➤ Controlled cord traction (CCT)
➤ Uterine massage
These are maintained through the following steps;
1. Just after delivery, palpate the mother’s abdomen to exclude the second baby.
2. Give 10 unit oxytocin intramuscularly.
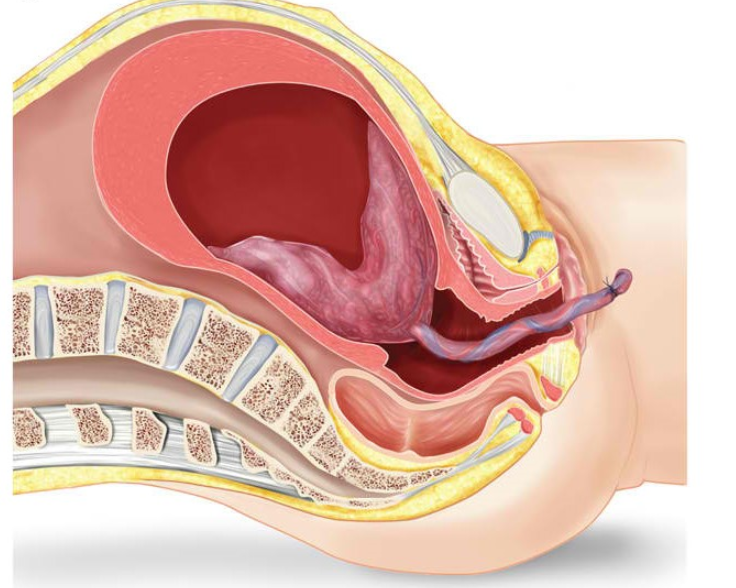
3. Clamp the cord close to the perineum with forceps.
4. Use one hand to grasp the forceps.
5. Place other hand on mother’s abdomen, with the palm facing toward the mother’s umbilicus & gently apply pressure in an upward direction (counter traction).
6. Firmly apply traction to the cord, in a downward direction, using the hand that is grasping the forceps.
7. Apply steady tension by pulling the cord firmly & maintaining pressure.
8. When the placenta is visible at the vaginal opening, cup it in both hands.
9. Use a gentle upward & downward movement or twisting movement to deliver the membrane.
10. Place the placenta in a kidney tray.
11. Gentle massage the uterus & make sure that uterus is well contracted.
Or (Another answer)
Management of Third Stage of Labour:
Third stage is the most crucial stage of labour. Previously uneventful first and second stage can become abnormal within a minute with disastrous consequences.
Steps of management:
A. Expectant management (traditional management):
➤ Psychological support to the mother
➤ Monitoring maternal pulse and BP
➤ Delivery of the baby
➤ Clamp, divide and ligate the cord
➤ Wait and watch
➤ Catheterization of the bladder
➤ Guard the fundus
➤ Separation of placenta
➤ Wait for spontaneous expulsion with the aid of the gravityastaviloba rotor alt 2
➤ If fails, assisted expulsion is done by
➤ Injection Oxytocin 5-10 units slowly IV or IM
➤ If fails, controlled cord traction (CCT) and fundal pressure
➤ Examiantion of the placenta, membranes and cord
➤ Inspection of the vulva, vagina and perineum is done.
B. Active management:
a) Principle:
The underlying principle in active management is to excite powerful uterine contractions within one minute of delivery of the baby (WHO) by giving parenteral oxytocic. This facilitates not only early separation of the placenta but also produces effective uterine contractions following its separation
The advantages are –
➤To minimise blood loss in third stage approximately to 1/5th and
➤ To shorten the duration of third stage to half.
b) Procedure:
➤ Inj. oxytocin 10 units IM (preferred) or methergin 0.2 mg I/M is given within one minute of delivery of the baby (WHO)
➤ The placenta is expected to be delivered soon following delivery of the baby
➤ If the placenta is not delivered thereafter, it should be delivered forthwith by controlled cord traction (Brandt-Andrews) technique after clamping the cord while the uterus still remains contracted.
➤ If the first attempt fails, another attempt is made after 2-3 minutes failing which another attempt is made at 10 minutes
➤ If this still fails, manual removal is to be done. Oxytocic may be given with crowning of the head, with delivery of the anterior shoulder of the baby or after the delivery of the placenta.
➤ If it fails again then placenta should be removed manually
[N. B. Controlled cord traction:
Upwards & backwards traction of the uterus with radial border of the hand over the symphsis and cord traction is given in a downward and forward direction.]
Nursing considerations:
Care of the Woman in the Third and Fourth Stages of Labor:
Nursing interventions:
– Administer oxytocin (IM or IV
– Inspect delivered placenta
– Monitor vital signs (q 15 minutes)
– Palpate fundus
– Observe character and amount of lochia
Non Pharmacologic Pain relief
-Relaxation
-Focusing on imagery
-Support from a doula or coach
-Breathing techniques
-Bathing/ hydrotherapy: C/I in ruptured membranes
-Therapeutic touch and massage
-Hypnosis: deep form of relaxation
-Biofeedback: based on belief that people can control and
-regulate internal events like HR and pain response
-Acupressure and acupuncture
-Heat or cold application
Pharmacologic pain relief
-Local infiltration
-Pudendal nerve block
-Spinal anesthesia
-Epidural anesthesia
Complication of Third Stage of Labour:
1. PPH due to –
➤ Uterine inertia
➤ Maternal injury
➤ Retained placental bits
2. Retained placenta
3. Uterine inversion
4. Obstetric inversion
5. Obstetric shock
6. Pulmonary embolism (amniotic fluid/air embolism)
Define of Lochia
Lochia:
In the field of obstetrics, lochia is the vaginal discharge after giving birth (puerperium) containing blood, mucus, and uterine tissue.
Or
It is the vaginal discharge for the first fortnight during puerperium.
Discharging sites:
Form uterine body, cervix and vagina.
Odor & reaction:
Offensive fishy smell & alkaline in react.
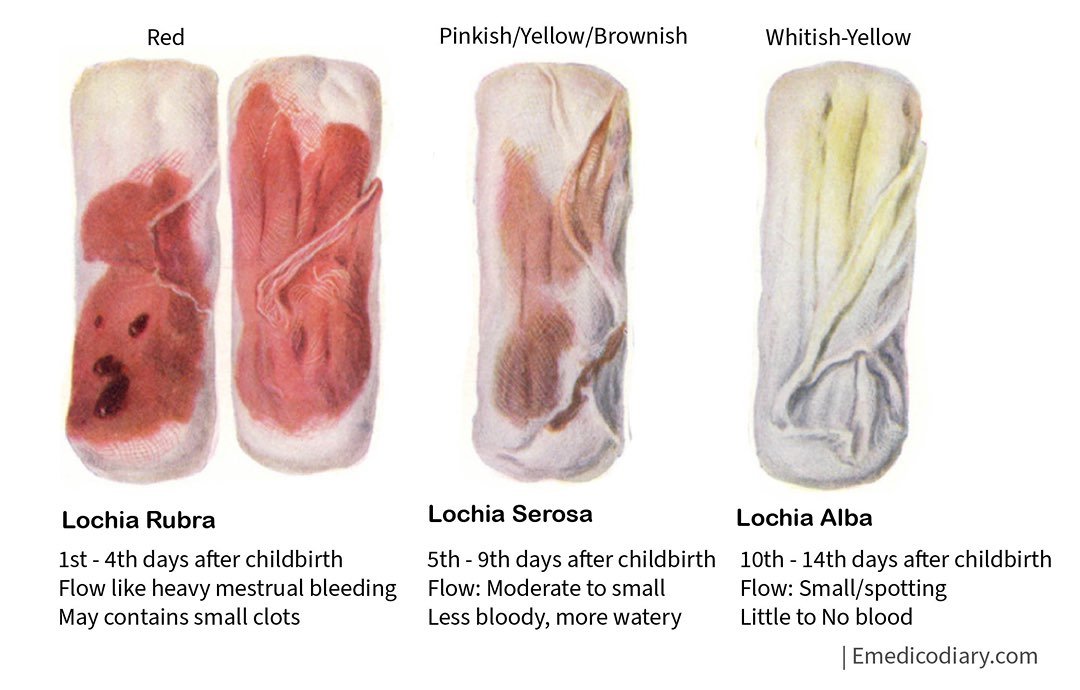
Types and colour: 3 type:
1. Lochia rubra (red) 1-4 days: Lochia rubra (or cruenta) is the first discharge, Composed of blood, shreds of fetal membranes, decidua, vernix caseosa, lanugo and membranes. It is red in color because of the large amount of blood it contains. It typically lasts no longer than 3 to 5 days after birth.
2. Lochia serosa & (yellowish) 5-9 days: Lochia serosa is the term for lochia that has thinned and turned brownish or pink in color contains serous exudate, erythrocytes, leukocytes, cervical mucus and microorganisms. This stage continues until around the tenth day after delivery. Lochia serosa which persists to some weeks after birth can indicate late postpartum hemorrhaging, and should be reported to a physician.
3. Lochia albs (pale white) 10-15 days: Lochia alba (or purulenta) is the name for lochia once it has turned whitish or yellowish-white. It typically lasts from the second through the third to sixth weeks after delivery. It contains fewer red blood cells and is mainly made up of leukocytes, epithelial cells, cholesterol, fat, mucus and microorganisms. Continuation beyond a few weeks can indicate a genital lesion, which should be reported to a physician.
Amount:
The average amount of discharge for the first 5-6 days is estimated to be 250 ml.
Clinical Importance of lochia:
The character of lochial discharge gives useful information about the abnormal puerperal state –
a. Odor: If offensive indicates infection.
b. Amount: Absent, scanty or excessive indicates infection.
c. Colour: Persistence of red color beyond the normal limit signifies sub-involution orretained bits of conceptus.
d. Duration: Duration of lochia albs beyond 3 weeks suggests local genital lesion.