Thomas Splints – An orthopedic nurse is a nurse who specializes in treating patients with bone, limb, or musculoskeletal disorders. Nonetheless, because orthopedics and trauma typically follow one another, head injuries and infected wounds are frequently treated by orthopedic nurses.
Ensuring that patients receive the proper pre-and post-operative care following surgery is the responsibility of an orthopedic nurse. They play a critical role in the effort to return patients to baseline before admission. Early detection of complications following surgery, including sepsis, compartment syndrome, and site infections, falls under the purview of orthopedic nurses.
Thomas Splints
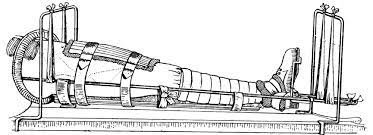
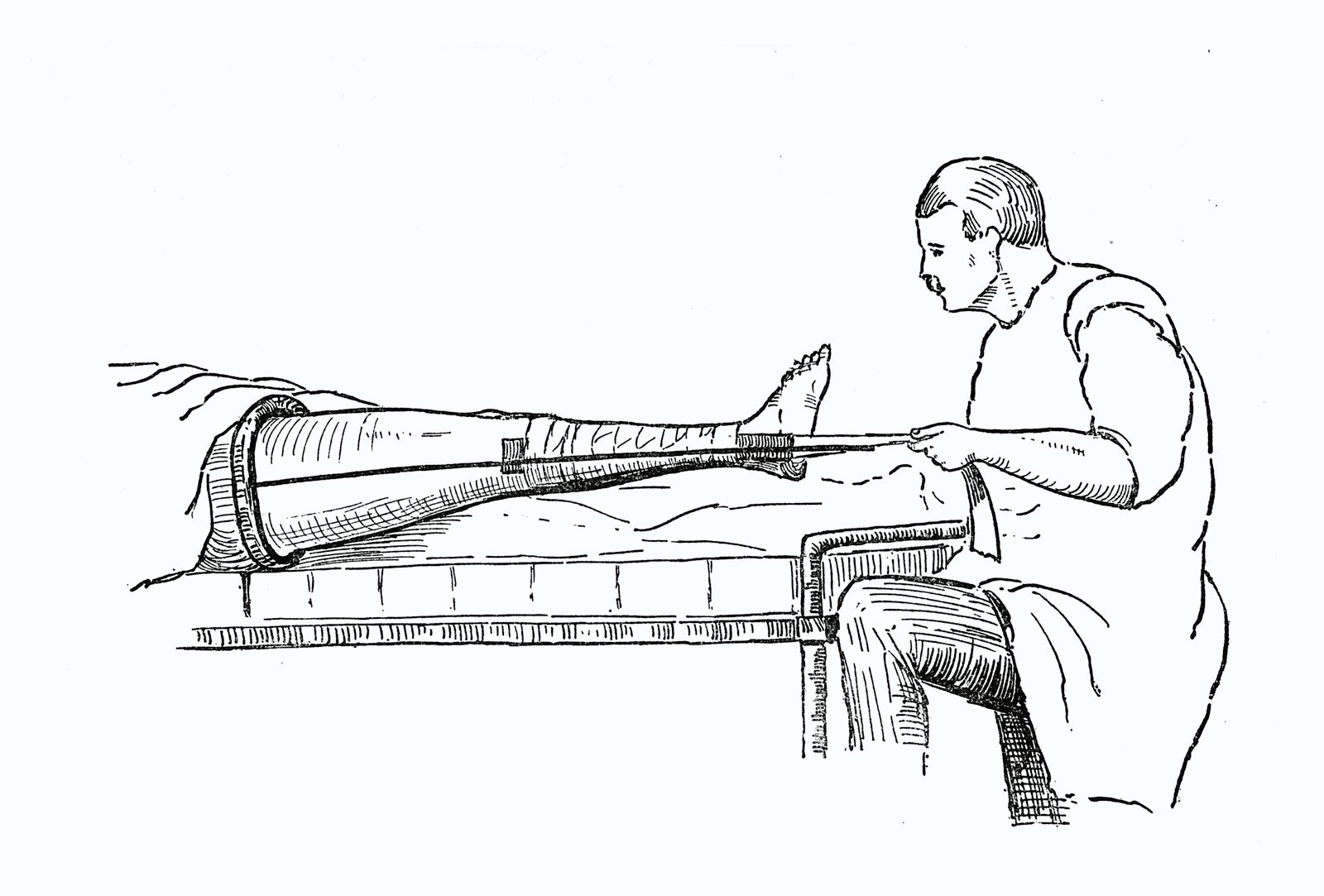
This is one of the very commonly used splints used in ortopaedics descrived by Hugh Owen Thomas in 1876 to assist for ambulatory treatment of TB knee. It is now widely used for the fracture of shaft of femur fracture.
Parts of Thomas splints:
A Thomas splint consist of 4 parts.
A padded metal oval rings.
Two sides bar: One inner and another outer bars of equal length.
Distal end: Where the two side bars are joined in the form.
Outer side bar: Is angled 2 inches below the padded ring to clear the prominent greater trochanter.
(Ref- BT.Basavanthappa, Orthopedics for nurses, 1″ edition, P-117)
Uses of Thomas splints:
1) To immobilize fracture of femur anywhere.
2) As a first aid measures.
3) For a transportation of injured patients.
4) In the treatment of joint disease. e.g- TB of knee.
(Ref- BT.Basavanthappa, Orthopedics for nurses,l” edition, P-117)
Nursing care for splint:
1. Patient must be kept in bed with comfortable position & small pad placed under the knee.
2. A pillow is place under the splint to support the limb.
3. The skin area under the Thomas splint must be always kept clean & dry.
4. The patient should be taught how to move the skin, under the ring every hour & encouraged to do this w himself.
5. Talcum powder may be used lightly under the pressure area..
6. Non absorbable cotton, wool may be use at the time uses of bed pan.
7. The patient is usually allowed more latitude in moving on bed.
9. Daily bath is given, the area of skin which was contact by the ring & the leather ring itself must have special care.
10. The patient may be turned toward the leg in the splint.
11. Thomas splint is frequently checked, if balance traction is applied.
12. Pressure in the groin & on the anterior, aspect of the thigh is prevented b> using a properly fitting splint. Maintaining adequate counter traction & placing a correct amount of weight.
13. Vital sign-symptoms will be checked & record on a chart.
14. Help to maintain personal hygiene.
15. Adequate fluid & nutrition diet will be given.
16. Bholer-Braun (BB) Splint.
B. Splints consist of 4 pulleys.
1) Proximal pulley prevents foot drops.
2) 2nd pulley to apply traction in the line of femur.
3) 3th pulley to apply traction in the line of supracondylar area of femur.
4) 4th pulley to apply traction in line of the legs.
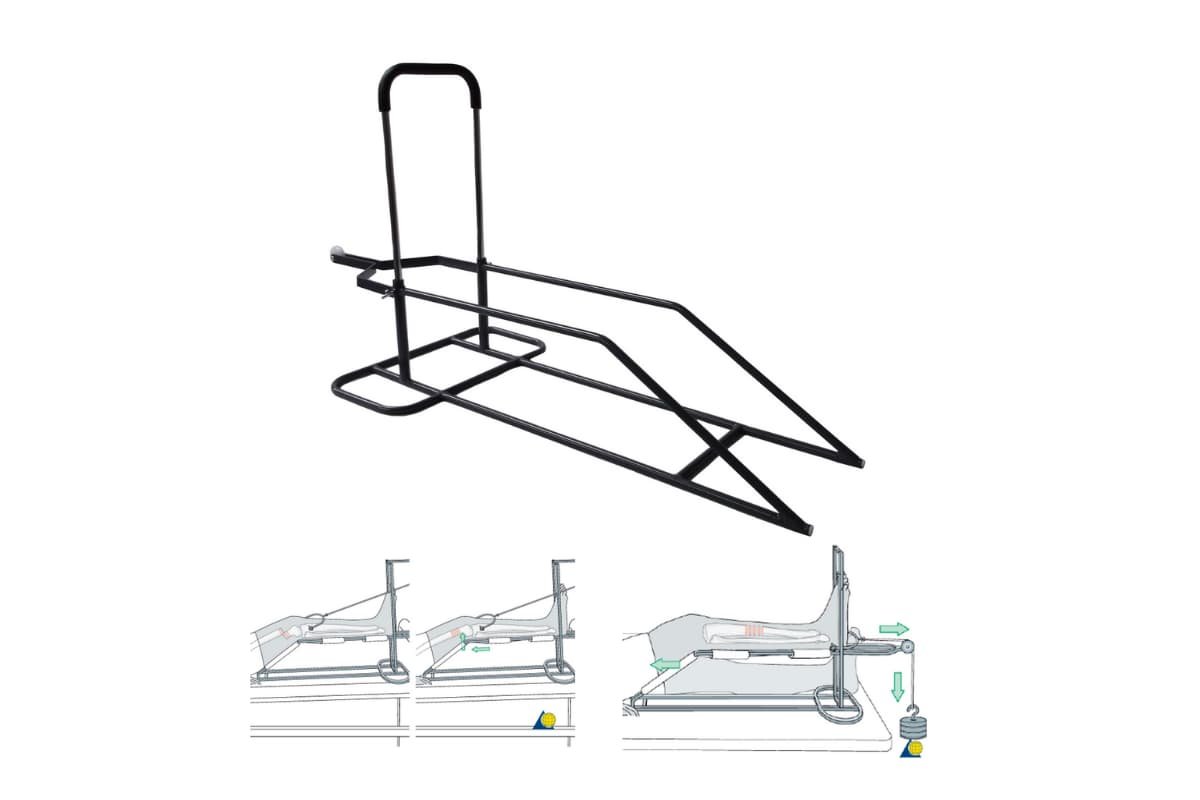
Indication of BB splints: Skeletal traction is applied through this frame for-
1. Comminuted trochanteric of femur.
2. Supracondylar of femur.
3. Shaft of tibia.
4. Shaft of fibula.
(Ref-John Ebnezar’s “Textbook of Orthopedics” 4″ edition,P-64)
Advantages of BB splints:
1. Mobile traction-especially useful in cases where transportation is necessary as the thraction unit I self contained
2. Limb in comfortable position
3. Wound care possible
4. Multipurpose application
5. Angle of traction can be changed by changing the pulleys [no change in arrangement required
6. Simultaneous traction through Calcaneal/diatal tibia and proximal tibia/distal femur can be given

Disadvantages & complications:
1) Nursing care is difficult.
2) It is very heavy and cumberosome frame.
3) It is associated with recumbent problems like bedsores, hypostatic pneumonia, renal calculi. Etc.
4) Non ambulatory
5) Stiffness/contracture
6) Urination and defecation becomes difficult
7) Common peroneal nerve compression
8) Other complications of recumbancy like bed sore, hypostatic pneumonia etc

(Ref-John Ebnezar’s “Textbook of Orthopedics” 4″ edition,P-65)
Precautions or regular monitoring is needed for patient in traction: 5 P’s-
1. Pulse and pins and needles Distal Neurovascular status atus sensations, distal pulsation, nailbed circulation, pain on passive dorsiflexion sign of compartment syndrome.
2. Pressure sores-heel, ischium and other pressure areas
3. Pin tract Infection detect early signs like pain, swelling, redness, discharge.
4. Physiotherapy ankle mobilization to prevent equinus, anti foot drop spilnt at nights. Knee and other joints mobilized if possible. Static quadriceps to be encouraged
5. Portable radiograph biweekly or as and when required in first 2 weeks and then weekly. Accordingly arrange the weight and direction of traction.
Preparation of the bed and setting up Bohler- Braun frame:
1. Attach canvas slings to the Bohler- Braun,
2. Prepare the upper leg with traction tapes and wrape the lower leg with traction tapes or a traction splint for skin traction and a pin /wire through the tibia or femur for skeletal traction.
3.Lift the injured leg and place the frame under the leg with the knee directly over the angle of frame.
4. Adjust the slings so that any pressure points are eliminated.
5. Tie traction cord to the spreader block and footplate, or splint, thread through the pulleys and then tie to the weight carriers. 6. Gently apply weights as prescribed by the physician
(Ref-Lippincott, Adult orthopaedic Nursing,P-122)
Read more: