Thyroid Pharmacology – This book covers the entire syllabus of “Pharmacology” prescribed by BNMC- for diploma in nursing science & midwifery students. We tried to accommodate the latest information and topics. This book is an examination setup according to the teachers’ lectures and examination questions.
At the end of the book, previous questions are given. We hope in touch with the book students’ knowledge will be upgraded and flourish. The unique way of presentation may make your reading of the book a pleasurable experience.
Thyroid Pharmacology
The thyroid gland secretes 3 hormones-thyroxine (T4), triiodothyronine (T3) and calcitonin. The former two are produced by thyroid follicles, have similar biological activity and the term ‘thyroid hormone’ is restricted to these only.
Synthesis:
The steps of thyroid hormone synthesis are as follows –
Site of synthesis: Colloid.
Raw materials:
1.Iodine
2. Tyrosine (each thyroglobulin contain 70 tyrosine).
Site of storage: Thyroglobulin (TG).
Steps:
➤Synthesis of thyroglobulin: Thyroglobulin is synthesis in the basal portion of follicular cell & secreted into the colloid.
➤Iodide trapping (Iodide pump): Active transport of I from blood into follicular cells through the basal membrane is called iodide pump.
➤Oxidation of iodide: Iodide ions are converted into oxidized form of iodine. Then iodine enters into the colloid.
➤Organification: Iodination of tyrosine at position 3 on the thyroglobulin ring and then on position 5 as well, forming mono iodotyrosine (MIT) at first and di-iodotyrosine (DIT) in the second.
➤Coupling: Coupling of iodinated tyrosine.
➤Storage: Each TG molecule contains up to 30 thyroxin molecules and a few T3 molecules. In this form, thyroid hormones are stored in the follicles in an amount sufficient to supply the body for 2-3 months.
➤Secretion: At first, thyroid cells uptake TG containing T3 & T4 by pinocytosis. Proteases digest the TG molecule and T3 & T4. The T3 & T4 the diffuse out of the thyroid cells and enter into the blood. The remaining TG is reused in the synthesis of hormones.
Storage of Thyroglobulin:
The thyroid gland has the ability to store a large amount of hormones.
After synthesis of the thyroid hormones, each thyroglobulin molecule contains up to 30 thyroxin molecules and a few triiodothyronine molecules. In this form, the thyroid hormones are stored in the follicles in an amount sufficient to supply the body with its normal requirements of thyroid hormones for 2 to 3 months. Therefore, if the synthesis of thyroid hormone is stopped, the physiologic effects of deficiency are not observed for several months.
Mechanism of action
Most of the hormone (T3 and T4) is bound to thyroxine-binding globulin in the plasma. The hormones must dissociate from thyroxine-binding globulin prior to entry into cells. In the cell, T4 is enzymatically deiodinated to T3, which enters the nucleus and attaches to specific receptors.
The activation of these receptors promotes the formation of RNA and subsequent protein synthesis, which is responsible for the effects of T4.
Pharmacokinetics
Both T4 and T3 are absorbed after oral administration. Food, calcium preparations, and aluminum-containing antacids can decrease the absorption of T4. Deiodination is the major route of metabolism of T4. T3 also undergoes sequential deiodination. The hormones are also metabolized via conjugation with glucuronides and sulfates and excreted into the bile.
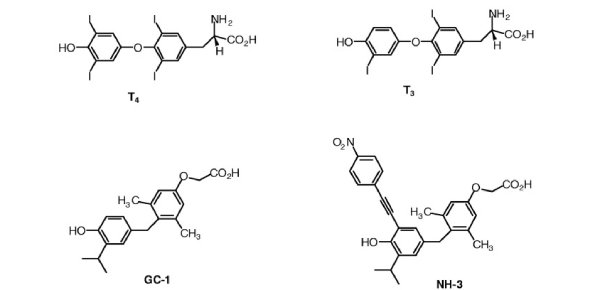
Differences between T3 & T4:
| Traits | T3 | T4 |
| 1. Amount of secretion | 7% | 93% |
| 2. Potency | 4 times more potent than T4 | Less potent |
| 3. Onset of action | Rapid | Slow |
| 4. Duration of action | Short, 2-3 days | Long, 6 wks to 2 months |
| 5. Plasma protein binding affinity | Less affinity | High affinity |
| 6. Release from plasma protein | 1 day | 6 days |
Abnormalities of Thyroid Functions
A. Hyperthyroidism (thyrotoxicosis):
- Diffuse toxic goitre
- Toxic nodular goitre
B. Hypothyroidism:
- Adult: myxoedema (reversible)
- Children: cretinism (ineversible)
- Simple non-toxic goitre due to iodine deficiency.
Hypo and Hyperthyroidism
Inadequate secretion of thyroid hormone (hypothyroidism) results in bradycardia, poor resistance to cold, and mental and physical slowing. In children, this can cause mental retardation and dwarfism.
In contrast, excess secretion of thyroid hormones (hyperthyroidism) can cause tachycardia and cardiac arrhythmias, body wasting, nervousness, tremor, and heat intolerance.
Hypothyroidism
Hypothyroidism, thyroid insufficiency, is relatively common in adults and associated with tiredness and lethargy, weight gain, intolerance to cold, dry skin, bradycardia and mental impairment. Children with hypothyroidism manifest delayed bone growth, whereas a deficiency in utero also results in mental retardation – this condition is known as cretinism.
Hashimoto’s thyroiditis is an autoimmune disease resulting in fibrosis of the thyroid gland. It is the most common cause of hypothyroidism and, like most autoimmune diseases, is more prevalent in women. Myxoedema is also immunological in origin, and represents the most severe form of hypothyroidism, sometimes causing coma. Thyroid-hormone resistance and reduced TSH secretion will also produce the symptoms of hypothyroidism.
The Management of hypothyroidism.
Levothyroxine
Thyroxine is given as levothyroxine sodium in maintenance therapy. It has a half-life of 6 days and a peak onset of 9 days.
Mechanism of action
Levothyroxine is converted to T3 in vivo.
Route of administration
Oral.
Indications
Hypothyroidism
Contraindications
Levothyroxine should not be given to people with thyrotoxicosis, and should be used with caution in those who have cardiovascular disease.
Adverse effects
Arrhythmias, tachycardia, anginal pain, cramps, headache, restlessness, sweating, weight loss.
Therapeutic regimen
The starting dose of levothyroxine sodium should be no greater than 100 µg daily (reduce in the elderly or those with cardiovascular disease) and increase by 25-50 µg every 4 weeks until a dose of 100-200 µg is reached.
Liothyronine sodium (L-triiodothyronine sodium)
As liothyronine is bound only slightly by thyroid binding globulin, it has a more rapid onset of effects and a shorter duration of action than levothyroxine.
Mechanism of action
Liothyronine is rapidly metabolized in vivo to T3. It has a half-life of 2-5 days and a peak onset of 1-2 days.
Route of administration
Oral, intravenous.
Indications
Liothyronine is given for severe hypothyroidism where a rapid effect is needed
Contraindications
Liothyronine should not be given to people with cardiovascular disorders
Adverse effects
Arrhythmias, tachycardia, anginal pain, cramps, headache, restlessness, sweating, weight loss.
Therapeutic regimen
The dosage of liothyronine sodium should be gradually increased as with levothyroxine sodium (20 µg liothyronine sodium is equivalent to 100 µg levothyroxine sodium). Intravenous liothyronine is the drug of choice in the emergency treatment of myxoedema (hypothyroid) coma.
Hyperthyroidism
Hyperthyroidism, thyroid excess, results either from the overproduction of endogenous hormone or exposure to excess exogenous hormone. Symptoms include increased basal metabolic rate (BMR) with consequent weight loss, increased appetite, increased body temperature, and sweating, as well as nervousness, tremor, tachycardia and classic ophthalmic signs.
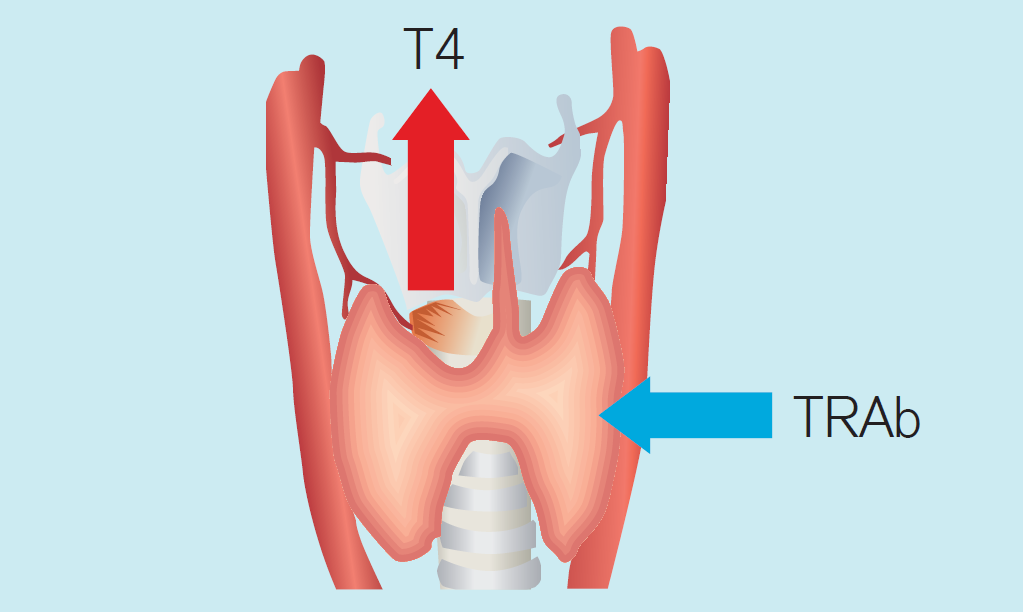
Graves’ disease (diffuse toxic goitre) is the most common cause of hyperthyroidism. It is an autoimmune disease caused by the activation of TSH receptors by antibodies. This results in an enlargement of the gland and therefore excess hormone production.
Toxic nodular goitre is the second most common cause of hyperthyroidism. It is due to either a single adenoma (hyperfunctioning adenoma) or multiple adenomas (multinodular goitre).