Tonsillitis and Tracheostomy – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Tonsillitis and Tracheostomy
Tonsillitis is an infection and swelling of the tonsils, which are ovalshaped masses of lymph glad tissue located on both sides of the back of the throat.
Or,
This is generalized inflammation of the facial tonsils and is caused by beta-hemolytic streptococcus, virus, staph, and pneumococcus
The Causative Organism:
The most common bacterial cause of tonsillitis is Group A beta-hemolytic streptococcus (GABHS).
a. Bacteria:
- Haemolytic streptococci
- Strep. pneumoniae
- Staphylococcus
- Haemophylus
b. Virus:
- Rhinovirus
- Adenovirus
- Enterovirus
Management of Acute Tonsillitis:
Clinical features:
➤ Symptoms:
- Sore throat – uneasiness or foreign body sensation during swallowing.
- Pain on swallowing.
- Pyrexia & malaise.
- Headache & earache.
➤ Signs:
- Temperature-102°F to 104°F.
- Increased pulse rate.
- Tonsils are enlarged & congested
- Tonsils studded with yellowish spot forming patches on tonsils.
- Furred tongue.
- Foetid breath-foul smelling breath due to pus.
- Enlarged, tender, jugulo-digastric lymph node or tonsillar lymph node.

Differential Diagnosis:
➤ Diphtheria.
➤ Scarlet fever.
➤Vincent’s infection.
➤ Agranulocytosis.
➤ Glandular fever.
➤ Oral thrush.
Investigations:
➤Throat swab for culture & sensitivity.
➤ Blood for TC & DC of WBC, ESR.
Treatment:
➤ General treatment:
- Bed rest.
- Soft diet.
- More fluid intake.
- Warm saline gurgling.
- Vitamin C is sometimes helpful.
- Tepid sponging.
➤ Specific treatment:
- Systemic antibiotics – Penicillin is the drug of choice.
- Oral Penicillin-250 mg every 6 hourly for 5-7 days.
- Amoxicillin 50 mg/kg body weight every 8 hourly for 5-7 days.
- Analgesics to relieve pain & antipyretics.
Nursing Management of Tonsillitis:
1. The patient should be provided bed rest
2. Monitoring vital signs and record it specially temperature.
3. Maintain isolation of the patient to prevent spread of infection.
4. Soft and liquid diet should be provided to the patient such as fruit juice, soup etc.
5. Some investigation such as throat swab C/S, blood for- TC, DC, ESR.
6. To maintain warm water gurgling, mouthwash with saline water or NaCO3.
7. To provide symptomatic care.
8. Acute management by medication according to doctor’s ordered
- Antibiotics: Inj. Cryst penicillin 5 Lacs twice in daily, Tab. Phenoxymethyl penicillin 250mg 6 hourly for 7 days
- For temp. & pain – Paracetamol 500mg thrice daily or soluble aspirin 300mg
- Warm water gurgling & mouthwash with saline water or NaCO3
- For constipation-milk of magnesium I tsf. thrice daily
- Soft diet & vit-‘C’ is given
9. Chronic management by medication according to doctor’s order
- Treatment is conservative at first with attention to general health, nutritional diet, well ventilated room, like that of acute tonsillitis
- If trouble persists & recurrent i.e. at least ¼ attacks in a year then tonsillectomy is advised
10. Advice the patient not to take too cold or hot foot.
11. To maintain regular oral hygiene
12. Encourage the patient to take nutritious diet
13. The patient is observed for postoperative complication
14. The patient have to be said to remove oral & nasal secretion to prevent infection
Complication of Tonsillitis:
- Peritonsillar abscess.
- Parapharyngeal & retropharyngeal abscess.
- Oedema of the larynx.
- Acute rheumatism.
- Acute nephritis.
- Acute infection of the middle ear cleft.
- Septicaemia.
- Chronic tonsillitis.’
Indications of Tonsillectomy Operation:
1. Recurrent attacks of tonsillitis (at least > 2 times for 2 consecutive years)
2. Hugely enlarged tonsils causing mechanical obstruction to swallow, breathing
3. Tonsil acts as a source of infection (may cause repeated TB adenitis, persistent carrier of diphtheria bacilli or streptococci haemolyticus)
4. Unilateral tonsillar enlargement producing suspicion of malignancy.
5. Previous attack of peri- tonsillar abscess
6. As a part of uvulo- palate- pharyngoplasty. (sleep apnoea)
7. For approach to enlarged styloid process
Contraindications:
1. Acute upper respiratory tract infection, LRTI
2. Bleeding or clotting disorders
3. Epidemic poliomyelitis
4. Severe systemic disorders:
- Severe DM
- Gross HTN
- Severe asthma
5. Acute tonsillitis
Post-Operative Management:
➤ Patient is returned to bed and is placed in tonsillar position, i.e. on the side with a pillow behind him, with knee & hip flexed
➤ Antibiotic: Inj. amoxicillin 500mg 8hourly for 5-7 days
➤ Nothing by mouth for first 5-6 hours
➤ Analgesic: Liquid paracetamol
➤ Then, sips of water in the evening
➤ Patient is encouraged to drink & eat soft solid diet from the nest day. Ice cream, cold milk, cold Horlicks may be given
➤ Antiseptic gurgle after each feeding with H₂20206
➤ Monitoring of the patient: pulse, BP, temperature, respiratory rate
Complications of Tonsillectomy Operation:
A. Per-operative:
a. Primary haemorrhage
b. Injury to the lips, gums, teeth ant, pillar, port, pillar, soft palate, pharyngeal wall
c. Pulmonary:
- Aspiration pneumonia
- Collapse
- Lung abscess. (late complication)
d. Anaesthesia: injury to vocal cord, larynx
B. Post-operative:
a. Reactionary haemorrhage (less than 1%)
b. Secondary haemorrhage. (after 5-7th post-operative day)
e. Infection:
- Cellulitis of neck
- Parapharungeal abscess
- Retro pharyngeal abscess
- Chest infection
C. Other complication:
- Acute otitis media
- Sepsis-spreading laterally may cause para-pharyngeal abscess and cellulitis neck
- Dental injury
- Posterior pillar and palatal injury
- Incomplete removal and recurrent tonsillitis
- Polio: may occur in the post-operative period during an outbreak of epidemic
Tracheostomy
Definition of Tracheostomy:
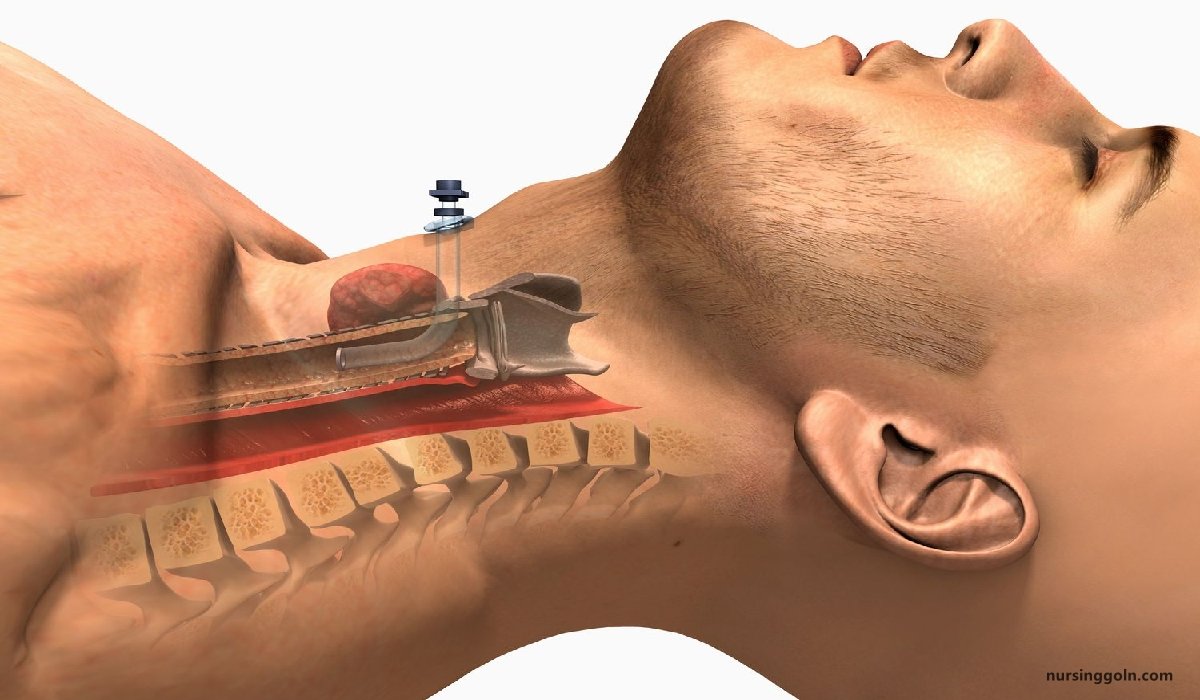
A tracheostomy is an opening surgically created through the neck into the trachea to allow direct access to the breathing tube and is commonly done in an operating room under general anesthesia
(Ref by: http://www.hopkinsmedicine.org)
Or,
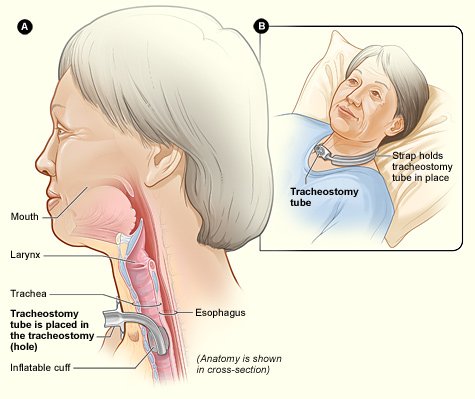
A tracheostomy is an artificial opening into the trachea, which is kept patent by the insertion of a metal or portex tube.
(Ref by-Margaret Clarke’s/11/178)
A tracheostomy describes the surgical procedure of creating an artificial opening in the trachea to relieve an obstruction of the airway. This artificial airway is maintained by a tube.
(Ref-SN Nanjunde Gowda’s/2nd/415)
Or,
A tracheostomy is an artificial opening made into the trachea through which a curve tube, called tracheostomy.
Definition of Tracheostomy Tube:
Tracheostomy tube is a small metal or plastic tube that keeps the stoma (opening) and the trachea in a tracheostomy open. Also known as a trach (pronounced ‘trake’) tube.
Types of Tracheostomy Tube:
1. Single Lumen Tubes
2. Double Lumen Tubes
3. Uncuffed Tubes
4. Cuffed Tubes
5. Fenestrated Tubes
6. Adjustable flange tubes
Or.
A. Emergency tracheostomy.
B. Elective tracheostomy.
a) Temporary tracheostomy.
b) Permanent tracheostomy.
(Ref by-Bailey & Love’s/25/718)
Importance/Purposes of Suctioning a Tracheostomy Tube:
1. To prevent damage of mucosal lining during suctioning.
2. Remove obstruction from the airway.
3. To make the safe of the life of patient.
4. To provide a method for mechanical ventilation of the patient.
5. To maintain airway potency.
6. To remove tracheobronchial secretions.
7. To promote cleanliness.
8. To prevent infection.
9. To prevent hypoxemia and hypoxia.
Indications of Tracheostomy:
Conditions that may require a tracheostomy include:
- Anaphylaxis
- Birth defects of the airway
- Burns of the airway from inhalation of corrosive material
- Cancer in the neck
- Chronic lung disease
- Coma
- Diaphragm dysfunction
- Facial burns or surgery
- Infection
- Injury to the larynx or laryngectomy
- Injury to the chest wall
- Need for prolonged respiratory or ventilator support
- Obstruction of the airway by a foreign body
- Obstructive sleep apnea
- Paralysis of the muscles used in swallowing
- Severe neck or mouth injuries
- Tumors
- Vocal cord paralysis
Complications of Tracheostomy:
| A. Intra operative complications: |
|
| B. Early postoperative complications: |
|
| C. Late postoperative complications: |
|
(Ref by-Bailey & Love/25/722)
Nursing Care Management for a Tracheostomy Patient:
A. Equipment
- Sterile disposable tracheostomy cleaning kit or supplies (sterile containers, sterile nylon brush or pipe cleaners, sterile applicators, gauze squares)
- Sterile suction catheter kit (suction catheter and sterile container for solution)
- Sterile normal saline (Check agency protocol for soaking solution)
- Sterile gloves (2 pairs)
- Cleari gloves
- Towel or drape to protect bed linens
- Moisture-proof bag
- Commercially available tracheostomy dressing or sterile 4-in. x -in. gauze dressing
- Cotton twill ties
- Clean scissors
B. Procedure:
1. Introduce self and verify the client’s identity using agency protocol. Explain to the client everything that you need to do, why it is necessary, and how can he cooperate. Eye blinking, raising a finger can be a means of communication to indicate pain or distress.
2. Observe appropriate infection control procedures such as hand hygiene.
3. Provide for client privacy.
4. Prepare the client and the equipment.
- To promote lung expansion, assist the client to semi-Fowler’s or Fowler’s position.
- Open the tracheostomy kit or sterile basins. Pour the soaking solution and sterile normal saline into separate containers.
- Establish the sterile field.
- Open other sterile supplies as needed including sterile applicators, suction kit, and tracheostomy dressing.
5. Suction the tracheostomy tube, if necessary.
- Put a clean glove on your no dominant hand and a sterile glove on your dominant hand (or put on a pair of sterile gloves).
- Suction the full length of the tracheostomy tube to remove secretions and ensure a patent airway.
- Rinse the suction catheter and wrap the catheter around your hand, and peel the glove off so that it turns inside out over the catheter.
- Unlock the inner cannula with the gloved hand. Remove it by gently pulling it out toward you in line with its curvature. Place it in the soaking solution. Rationale: This moistens and loosens secretions.
- Remove the soiled tracheostomy dressing. Place the soiled dressing in your gloved hand and peel the glove off so that it turns inside out over the dressing. Discard the glove and the dressing.
- Put on sterile gloves. Keep your dominant hand sterile during the procedure.
6. Clean the inner cannula.
- Remove the inner cannula from the soaking solution.
- Clean the lumen and entire inner cannula thoroughly using the brush or pipe cleaners moistened with sterile normal saline. Inspect the cannula for cleanliness by holding it at eye level and looking through it into the light.
- Rinse the inner cannula thoroughly in the sterile normal saline.
- After rinsing, gently tap the cannula against the inside edge of the sterile saline container. Use a pipe cleaner folded in half to dry only the inside of the cannula; do not dry the outside.
7. Replace the inner cannula, securing it in place.
- Insert the inner cannula by grasping the outer flange and inserting the cannula in the direction of its curvature.
- Lock the cannula in place by turning the lock (if present) into position to secure the flange of the inner cannula to the outer cannula.
8. Clean the incision site and tube flange.
- Using sterile applicators or gauze dressings moistened with normal saline, clean the incision site. Handle the sterile supplies with your dominant hand. Use each applicator or gauze dressing only once and then discard.
- Hydrogen peroxide may be used (usually in a half-strength solution mixed with sterile normal saline; use a separate sterile container if this is necessary) to remove crusty secretions. Check agency policy. Thoroughly rinse the cleaned area using gauze squares moistened with sterile normal saline.
- Clean the flange of the tube in the same manner.
- Thoroughly dry the client’s skin and tube flanges with dry gauze squares.
9. Apply a sterile dressing.
- Use a commercially prepared tracheostomy dressing of non-raveling material or open and refold a 4-in. x 4-in. gauze dressing into a V shape. Avoid using cotton-filled
gauze squares or cutting the 4-in. x 4-in. gauze. - Place the dressing under the flange of the tracheostomy tube.
- While applying the dressing, ensure that the tracheostomy tube is securely supported.
10. Change the tracheostomy ties.
- Change as needed to keep the skin clean and dry.
Post-Operative Nursing Care for a Tracheostomy Patient:
- Rest in bed.
- Patient should be kept in propped up position.
- Oxygen inhalation should be administered if needed.
- Suction.
- Humidification.
- Adequate fluid should be given.
- Administered antibiotic according to the doctor’s order to prevent infection.
- Analgesic if necessary.
- Monitoring vital signs.
- Wash of the inner tube by Sodium by carbonate solution 4 hourly.
- Calling bell, paper and pencil should be kept to the patient bed side.
Procedure of Suctioning a Tracheostomy Tube:
- Explain to the patient and their family that you are going to suction the tracheostomy tube.
- Hand hygiene
- Use personal protective equipment including non-sterile gloves and safety glasses.
- Suction using a clean, non-touch technique.
- Attach suction catheter to suction tubing
- Gently introduce the suction catheter into the tracheostomy tube to the pre-measured depth.
- Apply suction & gently rotate the catheter while withdrawing. Each suction should not be any longer than 5-10 seconds.
- Assess the patient’s respiratory rate, skin colour and/or oximetry reading to ensure the patient has not been compromised during the procedure. Repeat the suction as indicated by the patient’s individual condition.
- Rinse the suction catheter with sterile water decanted into bowl, not directly from bottle.
- Look at the secretions in the suction tubing they should be clear or white and move easily through the tubing.
- Notify the doctor if the secretions are abnormal, and consider sending a specimen for culture and sensitivity.
Dental Health
Definition of Dental Health:
According to WHO “Oral health is a state of being free from chronic mouth and facial pain, oral and throat cancer, oral sores, birth defects such as cleft lip and palate, periodontal (gum) disease, tooth decay and tooth loss, and other diseases and disorders that affect the oral cavity”.

Purposes of Maintaining Dental Health:
- To maintain socially acceptable & healthy life
- To prevent any kind of oral infection
- To keep the teeth healthy
- To protect the mouth from any kind of disease.
(Ref by-http://www.who.int)
Common Dental Problems in Bangladesh:
- Dental caries
- Discolor teeth
- Delayed eruption of teeth
- Calculus
- Sensitive teeth
- Bad breath
- Periodontitis
- Gingivitis
- Malocclusion of teeth
- Dental fluorosis
