Vesicovaginal Fistula (V.V.F) – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
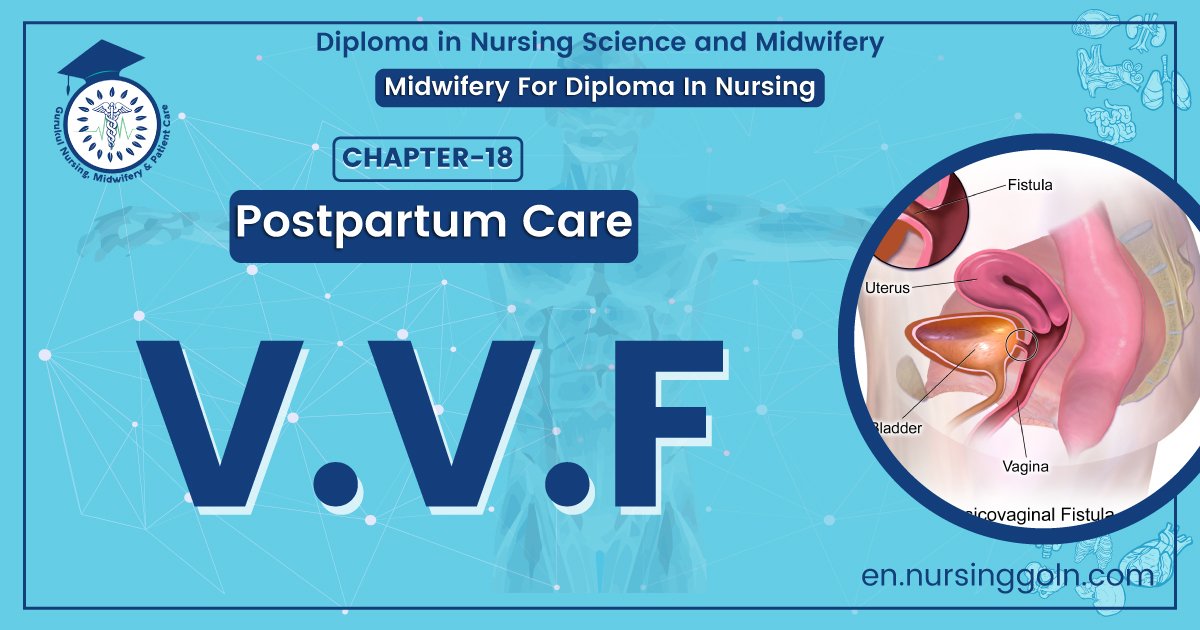
Vesicovaginal Fistula (V.V.F)
Definition
It means abnormal communication between the urinary bladder and the anterior vaginal wall This is the commonest type of genito-urinary fistula.
Causes of V.V.F
A. Congenital:
- Aberrant ureter: usually opens into vagina.
- Persistent urogenital sinus.
B. Acquired:
a. Obstetrical causetcommonest cause in our country
b. Prolonged obstructed labor: pressure by presenting part of fetus.
e. Forceps delivery.
d. Craniotomy.
e. Decapitation.
f. Lower segment caesarean section.۱۷۷
g. Rupture of previous lower segment operation scar.
h. Direct injury of ureter, bladder base or urethra by instruments,
C. Operative injury:
a. Hysterectomy: Abdominal/vaginal, Wartheim’s operation,
b. Fothergill’s operation.
c. Anterior colporrhaphy & sling operations.
d. Any operation involving anterior vaginal wall and urinary tract
D. Extension of disease process:
a. Carcinoma of cervix & vagina.
E. Infections:
a. Genitourinary tuberculosis,
b. Schistosomiasis (rare)
c. Lymphogranuloma venerium
d. Actinomycosis
F. Radiotherapy: as a late complication. Excessive, misapplied (accidental, interval radiotherapy into anteriorfornix) or even well applied irradiation in carcinoma cervix.
G. Accidents: Road traffic accidents causing crush injury to the pelvis.
H. Foreign bodies: Forgotten pessaries used for prolapse can erode vaginal wall by being impacted.
1. Chemical burns-
a. Douching.
b. Abortificientor
c. Quack treatment for prolapse can cause burning of urethra and anterior vaginal wall.
Mechanism of formation of obstetrical fistula
- During pregnancy, the bladder becomes an abdominal organ &
- Due to compression of urethra between the presenting part and symphysis pubis.
↓
The patient fails to empty the bladder.
↓
The urinary bladder walls get traumatized which may lead to blood stained urine, a common finding of in obstructed labour.
↓
The base of the bladder & urethra which are nipped in between the presenting part & symphysis pubis undergoes pressure necrosis.
↓
The devitalised tissue becomes infected & later on slough off
↓
Genito-urinary fistula; most commonly vesico-vaginal fistula or VVF

V.V.F is common in our country because
Obstetrical injury: commonest cause in our country.
a. Prolonged obstructed labor: pressure by presenting part of fetus.
b. Forceps delivery.
c. Craniotomy.
d. Decapitation.
e. Lower segment caesarean section.
f. Rupture of previous lower segment operation scar.
g. Direct injury of ureter, bladder base or urethra by instruments.
Operative injury
a. Hysterectomy: Abdominal/vaginal, Wartheim’s operation
b. Fothergill’s operation.
c. Anterior colporrhaphy& sling operations, iv. Any operation involving anterior vaginal wall and urinary tract
Diagnosis of V.V.E
A. Patient profile:
1. Patient gives history of difficult, obstructed labour or other relevant history, e.g. gynaecological operations or obstetric injury, malignancy of cervix, accidents or
radiotherapy.
2. Young pt
3. Low socio-economic condition
4. Short stature
B. Clinical feature:
1. Continuous dribbling of urine: true incontinence.
2. Absence of urge of micturation-
3. May have amenorrhoea.
4. Associated pruritus vulvae.
C. Signs:
General Examination-
- Usually these patient are short statured.
- Uriniferous odor from the patient.
- Wetling of the clothes or rubber sheet on the bed
Examination of vulva & perineum
- Vulva is moist, sored or ulcerated.
- Excoriation of vulva and perineum due to NH3
- Gushes of urine coming through vagina may be seen during coughing
P/V examination
- Speculum examination- Fistula is seen through which red bladder mucosa is seen.
- In dorsal position or Sim’s left lateral position-A large fistula is obviously seen.
Bimanual exam
- Fistula can be palpated by fingers. Metallic female catheter in urethra/bladder-tip can be seen or felt per vaginally
- This is done to determine the position: Mid, lower or upper vagina scarring
- Associated recto-vaginal fistula and complete perineal tear
Special tests
- If V.V.F is small, not easily visible or palpable-Three cotton swab test: Bladder is catheterised and methylene blue dye is introduced into the bladder. Three cotton swabs tare placed into vagina at different levels & seen whether they are wet with dye-If only the
lowest ball stains: urethro-vaginal fistula. - Middle & lower ball stain: VVF.
- If none of the balls stain but the upper one is wet: Uretero-vaginal fistula
Treatment of V.V.F
Conservative treatment:
- Worthwhile for small, recently formed WF, but can also be tried for fistula of several months.
- Continuous drainage of bladder by indwelling catheter for 21 days.
- Patient is kept in prone or sim’s position. Spontaneous healing occurs; If it fails, surgery is indicated.
B. Surgical treatment:
If conservative treatment fails, patient is asked to come after 3-6 months, so that in the meantime tissue reaction subsides, infection, local sepsis is eradicated, so repair operation is easy and easy healing occurs.
Type of operation:
Local repair by flap splitting method is the operation of choice.
1. Bladder wall by 2 layers
2. Vaginal wall by flap from labia majora.
Postoperative management:
1. Nothing by mouth till bowel sound return.
2. Continuous catheter drainage for 2-3 weeks.
3. Antibiotic- ampicillin
4. Advice on discharge-
- To check up after 6 weeks.
- To pass urine frequently.
- Take plenty of water and alkaline mixture for a few days. Avoid coitus for 3 months Avoid pregnancy for 2 years, (some teachers prefer for 3-6 months). The baby must be delivered by C/S.
- If family complete, advice ligation.
Prevention
A. Measures for obstetric cause:
a. Antenatal period:
Proper antenatal assessment for selection of cases. e,g. short stature, suspected CPD (cephalopelvic disproportion) and advice for hospital delivery.
Intra-natalperiod:
- Bladder emptied by catheter during labour or any operation.
- Prediction of prolonged labour and prevention of the same by labeling partograph chart.
- Cut short 2nd stage of labour by episiotomy or forceps.
Post-natal:
- Continuous self-retaining rubber catheter for 2-3 weeks gives rest to the bladder, improves circulation, prevents fistula or decrease the size if it has already occured.
- Antibiotic coverage, as there is already ischemic necrosis.
- Plenty of fluid intake.
- Prone/semi-prone position.
Surgical fistula:
- Proper identification of ureter & bladder during operation & care not to injure them.
- Catheterisation during hysterectomy & other gynaeological operations.
Cancer fistula:
- Early diagnosis and treatment of cancer cervix & vagina, o
- Prevention of Ca cervix by delaying the women’s age of marriage, and by delaying the age of first pregnancy.
- Exactly measured & exactly administered site of radiotherapy.
The criteria for local repair are
1. Small fistula.
a. Number is less, usually single.
- Site-not in bladder neck.
- Adequate tissue for mobilization.
b. Minimal loss of tissue.
- Adequate blood supply
Because, as a result of this catheterization-
- Size of fistula decreases – May be re-operable size.
- Small fistula may be healed up.
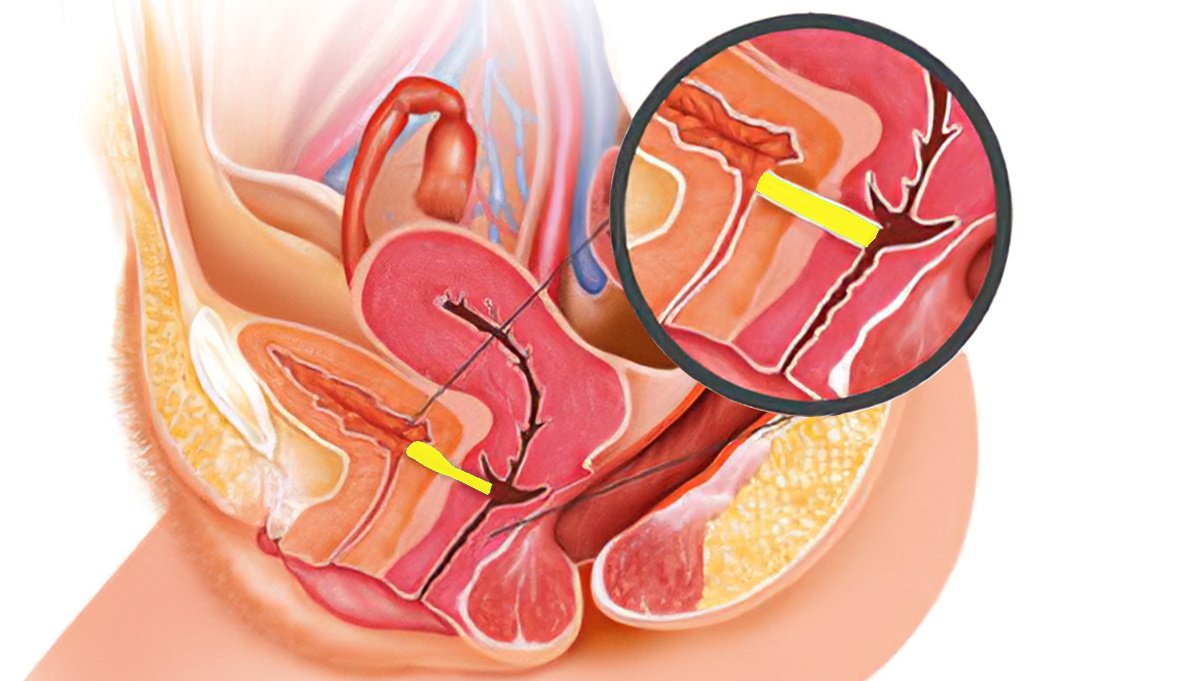
Definition
Recto-vaginal fistula can be defined as an abnormal communication between the rectum and the vagina lined by unhealthy granulation tissue.
Causes of RVF (Recto-vaginal fistula):
A. Obstetrical cause:
- Incomplete healing or unrepaired recent complete perineal tear, (commonest)
- Obstructed labour.
- Injury during destructive opt.
A. Operations:
- Posterior colpoperineiorrhaphy Repair of enterocele.
- Vaginal tubectomy Posterior colpotomy
- Reconstruction of vagina.
- Fall on sharp pointed object.
- Ca of vagina, cervix, bowel.
- Radiotherapy.
- Infection- vaginal TB, lymphovenereum.
- Crohn’s disease involving the anal canal or lower rectum.
- Chemical burn.
- Diverticulitis.
B. Congenital: The anal canal may open into the vestibule or in the vagina.
Management
Symptom: Involuntary escape of flatus and/or faeces into the vagina.
Sign: Recto-vaginal exam, reveals-
Faecal matter or faecalodour present in the vagina.
Fistula may be seen.
Tip of the metallic catheter may be seen or felt through vagina.
Investigation
1. Probe test: passing a probe through the vagina into the rectum.
2. Dye test: Methylene blue dye is introduced into the rectum which is seen escape out through the fistulainto the vagina.
3. Fistula due to partial healing of a complete tear: Make it into a complete tear & then repaired.
4. Fistula following obstructed labour:
- Bed rest, control of infection, nutritional support.
- Local repair by flap splitting method after 3 to 6 months.
- If traumatic: Repair immediately.
- Fistula following diverculitis: Resection of the affected loop of bowel and end to end anastomosis.
- Malignant state: Exenteration and colostomy.
- Following radiotherapy: Colpocleisis. (surgical closure of the vaginal canal)

Diagnosis
C/F:
- Escape of urine per vagina.
- Pt. has desire of micturation. INV:
- Three swab test.
- IVU.
Treatment: Uretero-neocystostomy.