Vulvular Heart Disease /Problems – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Vulvular Heart Disease /Problems
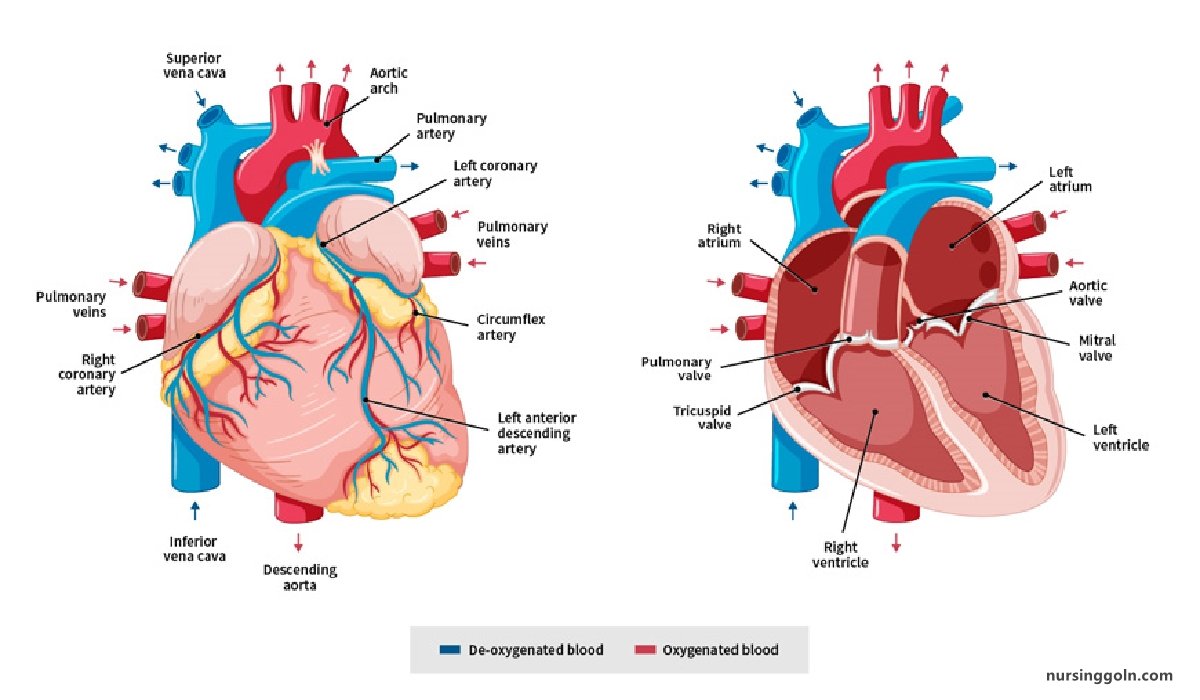
Mitral stenosis (MS) is characterized by obstruction to left ventricular inflow at the level of mitral valve due to structural abnormality of the mitral valve apparatus.
Causes of mitral stenosis:
- Rheumatic heart diseases (Principal cause)
- Calcification of mitral valve in elderly pt
- Congenital
- Lutembacher’s syndrome (Acquired MS with ASD)
(Ref: Davidson-234/518)
Nice to know:
- Normal mitral orifice: 5 cm³. (4-6 cm³)
Classification of MS according to mitral valve orifice:
- Minimal: mitral valve area <5 but >2.5 cm²
- Mild: mitral valve area 1.5 to 2.5 cm²
- Moderate MS: 1-1.5 cm³
- Severe MS/critical MS: < 1 cm² Symptoms at rest.
Clinical feature:
Symptom:
- Breathlessness (due to pulmonary congestion)
- Fatigue (due to low cardiac output)
- Oedema, ascites (right heart failure)
- Palpitation (atrial fibrillation)
- Haemoptysis (due to pulmonary congestion, pulmonary embolism)
- Cough (due to pulmonary congestion)
- Chest pain (due to pulmonary hypertension)
- Symptoms of thromboembolic complications (e.g. stroke, ischaemic limb)
Signs
- Pulse- irregularly irregular pulse (Atrial fibrillation)
- Mitral facies (Malar flush)
- JVP-Raised JVP if developed right heart failure
- Palpation
✔ Tapping apex beat
✔ Palpable P2 if develops pulmonary hypertension
✔ Left parasternal heave if rt. ventricular hypertrophy.
- Auscultation:
✔ Loud 1″ heart sound, opening snap
✔ Mid-diastolic murmur (there is a localized low pitched, rough, rumbling, mid diastolic murmur preceded by an opening snap with a pre-systolic accentuation without any radiation best heard by the bell I of the e stethoscope over the mitral area patient in left lateral position breath hold after expiration)
- Signs of raised pulmonary capillary pressure:
✔ Crepitations, pulmonary oedema, effusions
Investigations of mitral stenosis:
- ECG:
✔ Left atrial hypertrophy (P mitrale)
✔ Right ventricular hypertrophy (Tall R wave in V1,V2 & deep S wave in Vs, V6),
✔Feature of Atrial fibrillation
- Chest X-ray:
✔ Enlarged left atrium with appendage
✔ Signs of pulmonary venous congestion
- Echo
✔ Thickened immobile cusps
✔ Reduced valve area han di
✔ Reduced rate of diastolic filling of LV Enlarge left atrium
- Doppler
✔ Pressure gradient across mitral valve
✔ Pulmonary artery pressure
✔ Left ventricular function
- Cardiac catheterization: Assessment of coronary artery disease, pulmonary artery pressure
- MS and MR
Treatment
- Medical treatment: [Remember = ADDA]
✔ Anti-coagulants: Warfarin
✔ Pt with systemic embolization for at least 1 yr.
✔ Pt with atrial fibrillation for permanently
✔ Ventricular rate control by Digoxin: 0.25 mg/day, beta blocker or calcium channel blocker in artial fibrillation.
✔ Diuretics to control pulmonary congestion & rt. heart failure,
✔ Prophylactic antibiotic against infective endocarditis (rarely recommended)
- Definitive treatment:
✔ Mitral balloon valvuloplasty: treatment of choice.
✔ Mitral valvotomy-if facilities or expertise for valvuloplasty are not available,
✔ Mitral valve replacementat
- Monitoring & after care:
✔ Echocardiography
✔ ECG
✔ Follow up: 1-2 yearly
(Ref by: Davidson-517-18/234)
Complications of Mitral Stenosis:
- Atrial fibrillation.all
- Systemic thrombo-embolism eg. Stroke, gangrene of limbs, intestine.
- Pulmonary HTN.
- Right heart failure,
- Pulmonary infarction
- Chest infection
- Tricuspid regurgitation.
- Infective endocarditis.
- Haemoptysis
- Ortner’s syndrome (Hoarseness of voice due to compression of left laryngeal nerve)
- Dysphagia (Due to oesophageal compression)
(Ref-Kumar & clark-760/8)
Radiological Findings in Mitral Stenosis:
i. Signs of enlarged left atrium
- Fullness of pulmonary conus leads to straightening of left heart border,
- Double contour of rt heart border.
- Upper lobe diversion
- Widening of carina.
- Left bronchus appears horizontal.
ii. Signs of pulmonary venous congestion
- Kerly’s B lines..
- Ground glass appearance.
iii. Calcified mitral valve may be seen in the late course of disease on a penetrated or lateral view
(Ref-Kumar & clark-742/8)
Differences mitral stenosis from aortic regurgitation:
| Traits | Mitral stenosis | Aortic regurgitation |
| 1. Pulse | Low in volume & normal in rhythm. May be irregularly irregular (if AF). | High volume, collapsing pulse. |
| 2. Blood pressure | Normal | Wide pulse pressure.. |
| 3. Face | Malar flush. | Normal face |
| 4. Apex beat | Tapping. | Thrusting non sustained |
| 5. 1st heart sound | Loud | Normal |
| 6. Cardiac murmur | Mid-diastolic murmur at apex. | Blowing early diastolic murmur in left parasternal border at 3rd or 4th |
| 7. Pistol shot murmur over femoral artery | Absent. | Present |
| 8. Capillary pulsation in nail beds | Absent. | Present |
Mitral Regurgitation
Mitral valve regurgitation also → called mitral regurgitation, mitral insufficiency or mitral incompetence is a condition in which the heart’s mitral valve doesn’t close tightly, allowing blood to flow backward in heart.
Causes of Mitral Regurgitation:
- Rheumatic heart diseases (Principal cause-50%)
- MI
- Mitral valve prolapse
- Ischaeemia/infarction of papillary muscle
- Dilatation of the LV & mitral valve ring (Coronary artery disease, cardiomyopathy)
- Damage to valve cusps & chordae (Infective endocarditis)
Acute Causes of Mitral Regurgitation:
Acute MI (Rupture of papillary muscle)
Infective endocarditis
Acute rheumatic fever
Trauma in chest
Cardiac surgery.
(Ref by: Davidson/234/519)
Management of Mitral Regurgitation.
Clinical Features of Mitral Regurgitation:
Symptoms:
- Dyspnoea (pulmonary venous congestion)
- Fatigue (low cardiac output)
- Palpitation (AF, increased stroke volume)
- Oedema, ascites (right heart failure)
Signs:
- Atrial fibrillation/ flutter
- Cardiomegaly – Displaced hyperdynamic apex beat.
- Apical pansystolic murmur + thrill
- Soft S1, apical S3
- Signs of pulmonary venous congestion (crepitations, pulmonary oedema, effusions)
- Signs of pulmonary hypertension and right heart, failure,
Ref: Davidson-234/521)
Investigations mitral regurgitation:
i. ECG
Left atrial hypertrophy (if not in AF)
Left ventricular hypertrophy
ii. Chest X-ray:
- Enlarged left atrium
- Enlarged left ventricle
- Pulmonary venous congestion
- Pulmonary oedema (if acute)
iii. Echo
- Dilated LA, LV
- Dynamic LV (unless myocardial dysfunction predominates)
- Structural abnormalities of mitral valve (e.g. prolapse)
iv. Doppler:
- Detects and quantifies regurgitation
v. Cardiac catheterization:
- Dilated LA, dilated LV, mitral regurgitation
- Pulmonary hypertension
- Coexisting coronary artery disease
Treatment of Mitral Regurgitation:
i. Medical Management:
- Diuretics
- Vasodilators, e.g. ACE inhibitors
- Digoxin if atrial fibrillation is present
- Anticoagulants if atrial fibrillation is present
- Antibiotic prophylaxis against infective endocarditis
ii. Surgery:
- Mitral valve replacement or repair
Complication of mitral regurgitation:
- Acute left ventricular failure
- Infective endocarditis
- Systemic embolism
- Atrial fibrillation.
AORTIC REGURGITATION
Aortic regurgitation (AR) is the diastolic flow of blood from the aorta into the left ventricle (LV). Regurgitation is due to incompetence of the aortic valve or any disturbance of the valvular apparatus (eg, leaflets, annulus of the aorta) resulting in the diastolic flow of blood into the left ventricular chamber.
Causes of Aortic Regurgitation:
i. Congenital:
- Bicuspid valve or disproportionate cusps
ii. Acquired:
- Rheumatic disease
- Infective endocarditis
- Trauma
- Aortic dilatation (Marfan’s syndrome, aneurysm, dissection, syphilis, ankylosing spondylitis)
(Ref by: Davidson-234/524)
Symptom & Signs of Aortic Regurgitation:
Symptoms:
i. Mild to moderate AR:
- Often asymptomatic
- Awareness of heart beat, “palpitations’.
ii. Severe AR:
- Breathlessness
- Angina
Signs:
Pulses:
- Large volume or collapsing’ pulse
- Low diastolic and increased pulse pressure
- Bounding peripheral pulses
- Capillary pulsation in nail beds – Quincke’s sign
- Femoral bruit (pistol shot) – Durozie’s sign
- Head nodding with pulse – de Musset’s sign
ii. Murmurs:
- Early diastolic murmur (best heard with the diaphragm in left 3rd 4th intercostals space with the pt. leaning forward and breath hold in expiration)
- Systolic murmur (increased stroke volume)
- Austin Flint murmur (soft mid diastolic)
iii. Other signs:
- Displaced, rocking apex beat (volume overload)
- Pre-systolic impulse
- 4th heart sound
- Pulmonary venous congestion (crepitation’s)
Investigations of Aortic Regurgitation
i. ECG:
- Initially normal, later LV hypertrophy and T-wave inversion
ii. Chest X-ray
- Cardiac dilatation, maybe aortic dilatation
- Features of left heart failure
iii. Echo:
- Dilated left ventricle
- Hyperdynamic left ventricle
- Fluttering anterior mitral leaflet
- Doppler detects reflux
iv. Cardiac catheterization (may not be required)
- Dilated LV
- Aortic regurgitation
- Dilated aortic root
Treatment of Aortic Regurgitation.
- Asymptomatic patients should also be followed up annually with echocardiography
- Rx according to underlying conditions such as endocarditis or syphilis.
- Systolic blood pressure should be controlled with vasodilating drugs such as nifedipine or ACE inhibitors.
- Antibiotic prophylaxis against infective endocarditis
- Treatment of heart failure-Salt restriction, digoxin, diuretics & ACE inhibitors.
Surgical treatment:
i.Aortic valve replacement is indicated if
- Symptomatic aortic regurgitation
- Asymptomatic pt with LV ejection fraction<55% or LV end diastolic dimention increase to ≥ 55 mm
- Acute severe AR
ii. Sometimes combined with aortic root replacement and coronary bypass surgery may be necessary such as Marfan’s syndrome
(Ref: Davidson-524/23)

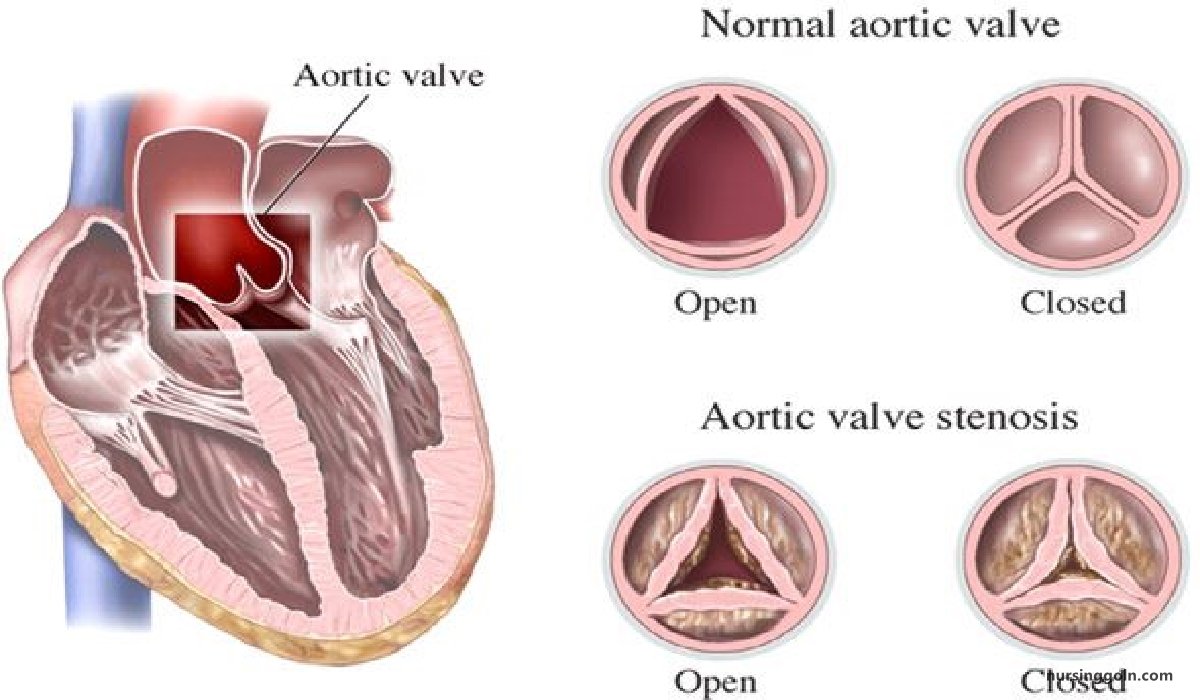
AORTIC STENOSIS
Aortic valve stenosis → or aortic stenosis occurs → when the heart’s aortic valve narrows. This narrowing prevents the valve from opening fully, which reduces or blocks blood flow from heart into the main artery to the body (aorta) and onward to the rest of the body.
Causes of Aortic Stenosis:
i. Infants, children, adolescents:
ii. Young adults to middle-aged:
- Calcification and fibrosis of congenitally bicuspid aortic valve
- Rheumatic aortic stenosis
iii. Middle-aged to elderly:
- Senile degenerative aortic stenosis
- Calcification of bicuspid valve
- Rheumatic aortic stenosis
Management of Aortic stenosis
Clinical feature of Aortic stenosis:
Symptoms:
- Mild or moderate aortic stenosis is usually asymptomatic
- Exertional dyspnoea
- Angina
- Exertional syncope
- Sudden death
- Episodes of acute pulmonary oedema
Signs:
- Ejection systolic murmur
- Slow-rising carotid pulse
- Narrow pulse pressure
- Heaving apex beat (LV pressure overload)
- Signs of pulmonary venous congestion (e.g. crepitations)
Investigations:
i.ECG:
- Left ventricular hypertrophy (usually)
- Left bundle branch block
ii. Chest X-ray:
- May be normal. Sometimes enlarged left ventricle and dilated ascending aorta on PA view, calcified valve on lateral view
iii. Echo:
- Calcified valve with restricted opening, hypertrophied LV
iv. Doppler.
- Measurement of severity of stenosis
- Detection of associated aortic regurgitation
v. Cardiac catheterization:
- Mainly to identify associated coronary artery disease
- May be used to measure gradient between LV and aorta
(Ref: Davidson/234/522-523)